Stock Footage Inc/Shutterstock
Hydroxychloroquine, the anti-malaria drug controversially touted as a cure for COVID despite a lack of robust evidence, is creating renewed interest as a potential treatment for omicron.
The discussion has been sparked by a new study from the University of Glasgow, which is yet to be published in a scientific journal, that looks at how antibodies from vaccines block omicron from entering cells. The researchers conclude, as many others have, that antibodies (the proteins that neutralise the virus) against previous variants or induced by vaccines are less effective against omicron. What’s interesting, though, is that the study finds that omicron may have changed the way it enters cells.
SARS-CoV-2, the virus that causes COVID, is coated in a lipid bilayer (a thin membrane made of two layers) just like our cells. When the virus enters our cells, the bilayers fuse like oil droplets on the surface of water, termed “membrane fusion”.
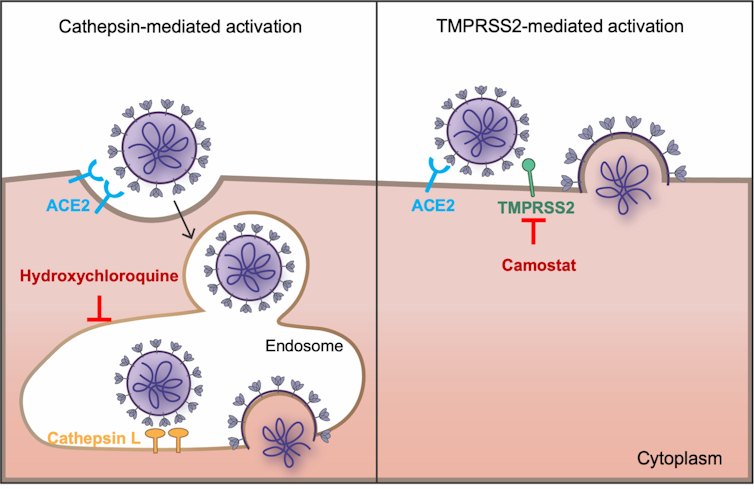
Membrane fusion occurs after the SARS-CoV-2 spike protein has attached to the ACE2 receptor on the cell surface, but can happen in two different places (see diagram below). Membrane fusion can occur on the cell’s surface, or it can can occur after the SARS-CoV-2 virus has been engulfed in an endosome.
The two ways coronavirus enters your cells
PLOS Pathogens, CC BY
An endosome occurs when the cell’s membrane folds back in on itself, creating a bubble of outside material inside the cell in order to take up nutrients. Normally the cell will then sort through the material and keep useful nutrients while discarding others. However, many viruses exploit endosomes as a way to enter cells.
This means that SARS-CoV-2 has two ways to enter cells: from the surface or via an endosome. The University of Glasgow study shows that omicron has picked up mutations that improve its ability to enter our cells via endosomes – and this is where hydroxychloroquine comes into play.
Hydroxychloroquine (HCQ) is a drug that accumulates in endosomes and decreases their acidity, which disrupts their function. Making endosomes less acidic reduces membrane fusion, thereby reducing SARS-CoV-2’s ability to enter cells. So HCQ could act as an antiviral.
This is possibly how HCQ acts as an anti-malarial and anti-inflammatory drug (although some researchers dispute this). It’s important to note that the new study does not test HCQ’s effect on omicron.
Hydroxychloroquine has had a difficult pandemic
HCQ has become notorious during the pandemic. The first study claiming HCQ is effective against COVID was criticised by science fraud expert Elisabeth Bik, who questioned the ethics, timelines for the trials, a lack of randomisation for patients and missing data.
Didier Raoult, the lead author of the work, then filed a criminal complaint against Bik for moral harassment, blackmail and extortion. During this, the French president, Emmanuel Macron, promoted HCQ – I assume in support of a fellow Frenchman, while use of the drug was also supported by Donald Trump, for reasons only clear to Donald Trump.
More bizarrely, a study published in the Lancet suggested that HCQ treatment actually increased fatalities, though this latter study has been accused of data fraud as well. Throughout all of this, other researchers have failed to find any positive benefits for HCQ, or strong indications for side-effects. HCQ has so far been an example of science at its worst.
But will hydroxychloroquine be effective against omicron? I struggle to see the benefits of treating omicron infections with HCQ. In the University of Glasgow study, the researchers show that omicron enters cells via endosomes more so than other variants, but they do not show that omicron is limited to using endosomes. It can still enter from the cell surface. Using HCQ to stop omicron entering via endosomes would therefore only marginally limit the virus from entering cells.
To show that HCQ is effective against omicron, scientists need to infect cells with omicron in the presence and absence of HCQ and shows a significant reduction in infectivity. If this shows that HCQ is effective against omicron, it would be sensible to test HCQ in a clinical trial.
However, unlike in March 2020 when HCQ was first suggested as a treatment, we have plenty of drugs to treat COVID including antivirals, such as molnupiravir and remdesivir, anti-inflammatories, such as dexamethasone, and antibody therapies.
![]()
Ben Krishna does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.











