The UK has passed the grim milestone of 100,000 deaths from COVID-19. And as the latest lockdown drags on, the inequalities that have characterised the trajectory of the COVID-19 epidemic are becoming starker than ever.
When coronavirus first arrived in the UK in spring 2020, British politicians called for teamwork and unity. It was proposed that COVID-19, as a “common enemy”, would align Britain and other nations like never before. “We are all in this together,” went the common refrain.
Broad messages of togetherness and cooperation are crucial for the success of public health campaigns – but they also imply that everyone is equally able to meet such expectations. Yet the UK’s demographic diversity means not everyone shares similar experiences during the pandemic. Far from it.
These are the issues my team is exploring at the Department of Behavioural Science and Health at University College London. Since March, we have been running the COVID-19 Social Study, which tracks the everyday experiences of more than 70,000 people around the UK through regular online surveys.
Every week we learn how people are feeling, how they are responding to restrictions, and what difficulties they are facing. We are gathering detailed information on everything from whether people are getting enough sleep to their risks of suffering loneliness.
Through studying these 70,000 people, we have found that someone’s experience of the crisis is largely dependent on their life situation prior to the lockdown. Our research shows that ethnic minorities, those who are financially vulnerable, those who come from lower socioeconomic positions and young people are struggling much more than those with greater social privilege.
This research supports the findings of other studies which show how COVID-19 has exacerbated societal inequalities, and it also identifies clear patterns of inequalities along racial lines.
This article is part of Conversation Insights
The Insights team generates long-form journalism derived from interdisciplinary research. The team is working with academics from different backgrounds who have been engaged in projects aimed at tackling societal and scientific challenges.
Our research highlights how crucial it is for the UK government to follow behavioural scientists’ insights into individual experiences. Rules to manage this virus and corresponding rhetoric and communications need to suit the realities of the public if we want to increase compliance and trust in authorities.
People are looking to leaders for guidance and solutions that are feasible and sensitive to their needs. But our findings show that, at the moment, this is not happening.
The unequal impact of lockdown
As we began to collect data in the first month of the UK lockdown, we immediately saw trends that suggested that people of lower socioeconomic position, or SEP, would struggle more.
Generally speaking, SEP refers to an individual’s position in society and their level of power or vulnerability given their resources. It depends on a range of factors, which in our studies include household income, educational qualifications, employment status, housing tenure and household overcrowding.
We found that those in low-income households and those who live in overcrowded conditions had less knowledge of COVID-19, felt less confident about accessing essentials such as food and medicine, and reported more factors that caused them stress.
One of our earliest studies on the topic supported these initial trends. It looked at 12,500 adults between March 25 and April 14. We gathered information on the number and types of difficulties people faced, how these related to their socioeconomic position, and how this changed during the first few weeks of lockdown.
We examined people’s financial stress: whether they or their partners had lost work or income and were struggling to pay bills; any difficulties regarding their basic needs such as food, medicine, and accommodation; and their experience of the virus, contracting it, or having someone close to them hospitalised or dying from it.
We found that there was a clear gradient across the number of adverse events experienced each week. Those who came from low SEP backgrounds experienced more adversity, particularly financial hardship and difficulties in accessing food and medication. This situation did not improve during the first few weeks of lockdown. Compared to those with higher SEP, people of low SEP were:
- 1.5 times more likely to report loss of work and twice as likely to report a partner’s loss of work
- 7.2 times more likely to be unable to pay bills, which increased to 8.7 times by the third week
- 4.1 times more likely to be unable to access sufficient food, increasing to 4.9 times in week three
- 2.5 times more likely to be unable to access required medication.
This suggests that efforts by the government to assist the public financially through furlough schemes or other initiatives did not go far enough – either not reaching the people who needed the most help in the first few weeks of the lockdown or being insufficient to properly address their adversities.
As the lockdown continued, we discovered that it had brought more hardship to those who were already struggling to live comfortably before the pandemic. By mid-July, it was apparent that, among those who found their financial situation very difficult before the lockdown, 57% reported that things were even worse. By November, this figure was 70%.
By contrast, only 20% of people who were living comfortably before the lockdown felt that they were worse off in November. About 27% of them actually said that their financial situation had improved due to reduced household spending, returns from investments, or directly profiting from financial opportunities provided by the pandemic. Only 7%-10% of people in difficult or very difficult financial situations reported an improvement during lockdown.
This has considerable policy implications for the UK’s current lockdown, with an end date that is uncertain. Stay-at-home orders disproportionately harm people who are already financially vulnerable, so lockdown provisions need to include more financial buffers or alternative financial options for people of low SEP if we want to avoid these inequalities widening further as this pandemic continues.
These financial solutions need to take account of the immediate hardship that people might face due to loss of work if they are forced to isolate, as well as the challenges they then might face finding future work in a challenging job market.
Poorer mental health overall
Early on in the crisis, researchers warned of two parallel epidemics: that of COVID-19, and one of poor mental health. This was concerning given that conditions such as anxiety and depression were already significant problems among the population – a quarter of adults are thought to have at least one diagnosable mental health problem per year.
We have tracked mental health since the beginning of the first lockdown in the UK. Our data shows that individuals’ mental health is affected not only by experiencing adversities such as financial strain, unemployment, and infection with the virus, but also by worrying about these consequences.
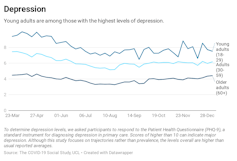
Mental health status is also driven by our work and living situations. Again, we found that SEP played a significant role in this. When we assessed symptoms of depression in the early weeks of lockdown, we found that low SEP was significantly associated with severe symptoms of depression.
Low household income, in particular, correlates with higher rates of depression and anxiety. Levels of anxiety and depression on average improved for adults in the UK across the first lockdown and the summer of 2020, but levels remained consistently higher among people with low household income.
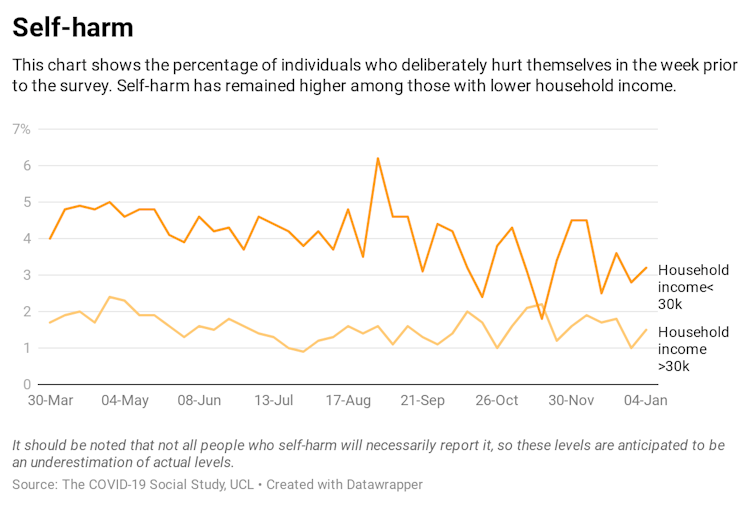
Throughout the first lockdown, low income was also consistently linked with more severe mental health issues, such as suicidal ideation and self-harm. Those suffering socioeconomic disadvantage or unemployment were also more likely to report physical abuse. However, such experiences have remained relatively stable throughout the period, making their relationship with the pandemic unclear.
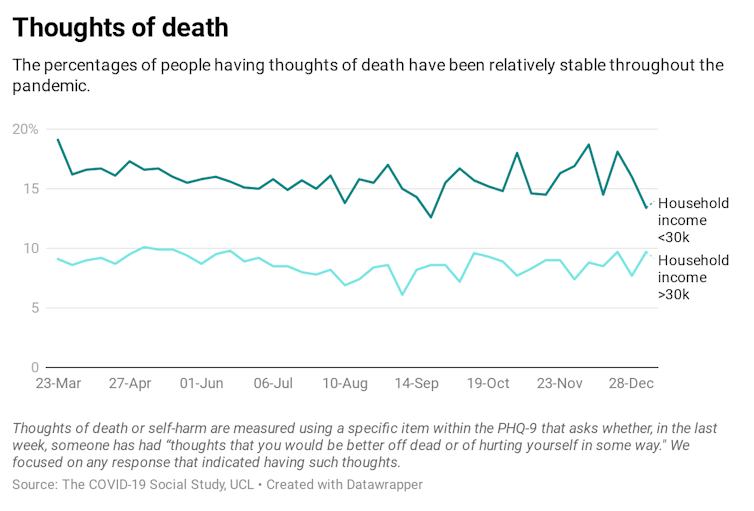
A relatively high proportion of people thought about death in general, which is unsurprising during a pandemic.
Mental health among ethnic minority groups
As we explored risk factors for poor mental health, we found clear inequalities not just in terms of SEP, but also according to ethnicity.
So far, our work has placed people in two groups: white ethnicity and those from black, Asian and other ethnic minority backgrounds. We recognise that this is not fully representative of the UK’s ethnic diversity and we intend to work on racial subgroups as the study progresses. However, with these groups in place, we have nonetheless been able to begin to unpack the disparities in experiences between white people and those from ethnic minority backgrounds.
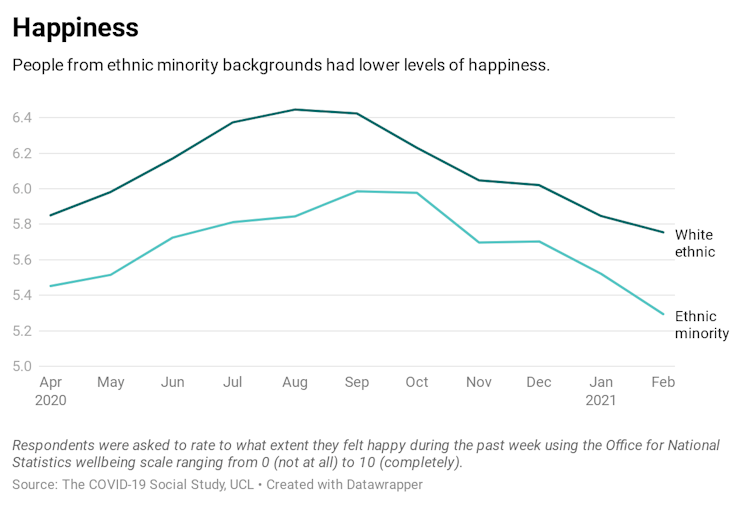
We have found that people from ethnic minority backgrounds have had poorer experiences across almost all measures in our study. These include confidence in the government and belief that health services could cope with the crisis, as well as depression, anxiety, stress, thoughts of death, self-harm, abuse, life satisfaction, loneliness and happiness.
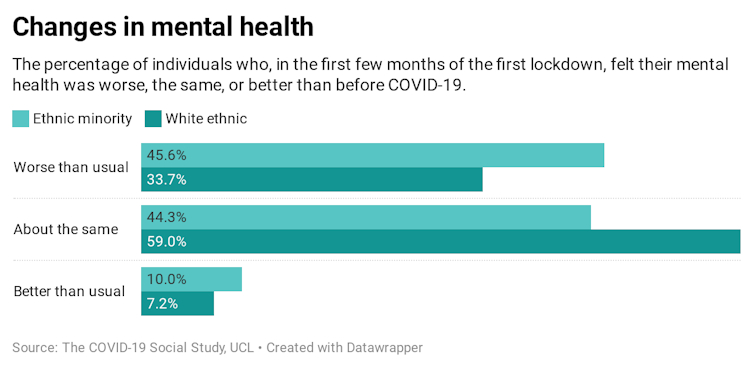
Among these, mental health stands out. About half of adults from ethnic minority backgrounds reported poorer mental health as a result of the pandemic. In comparison, only 35% of white participants reported worse mental health, indicating that ethnic minority groups experienced a disproportionate psychological burden. This has come in the form of anxiety, depression and low levels of life satisfaction, none of which have affected white people to the same extent.
Loneliness has also been higher for ethnic minorities: 23% often felt lonely compared to 17% of white people. Worries about unemployment and financial stress are also more common among ethnic minorities, of whom one in four reported such concerns. The ratio among white groups was half that.
In considering why we see these differences, there are two main explanations.
First, people from ethnic minority groups are disproportionately more likely to be of low SEP. Therefore they can experience the socio-economic burdens we have discussed above in higher levels to people of white ethnicity. Second, people from ethnic minority backgrounds have reported higher rates of being discriminated against across the pandemic – 42% of people experienced discrimination compared to 24% of people of white ethnicity.
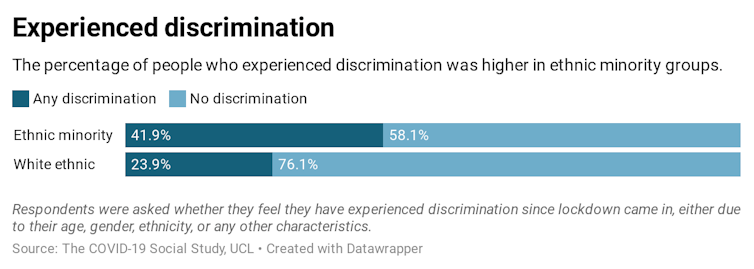
While discrimination could be for a range of reasons such as age, gender and disability, a large proportion of people from minority communities attributed their discrimination to ethnicity reasons. Given the worse levels of mental health, this is concerning, as higher levels of discrimination can act as triggers for depression, anxiety, and unhappiness.
Young people
A third key group to consider is young adults – those aged between 18 and 29. Since the start of the first UK lockdown, we have continued to collect data that demonstrates the discrepancies they face in mental health and wellbeing. Even before the pandemic, young adults were more likely to have poor mental health, and our findings indicate that the pandemic has exacerbated this.
In particular, young adults’ loneliness levels increased with the onset of the pandemic. The age group was already more likely than older people to feel lonely and this risk increased in the early months of the lockdown. Students, especially, were more at risk of loneliness than before the lockdown. For six weeks, levels did not improve and only by mid-May did we begin to see a slight decline in feelings of loneliness. As things stand, this age group continues to be the most lonely.
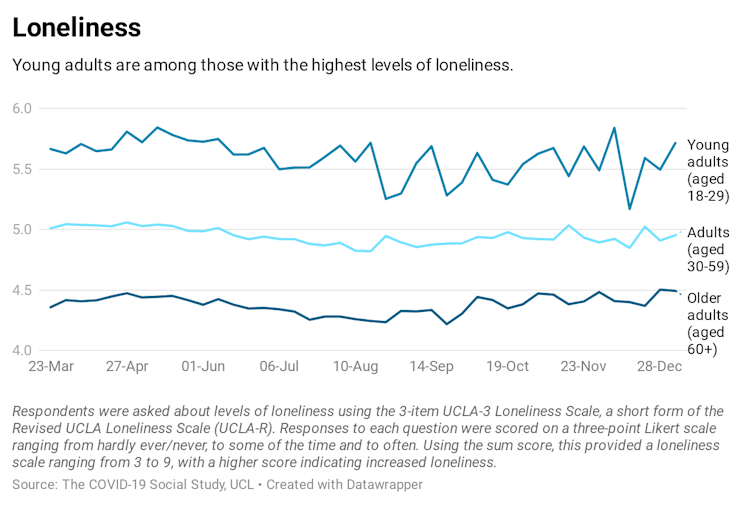
Young peoples’ levels of anxiety and depression have also been significantly higher.
In the first 20 weeks of lockdown there was gradual improvement, but it is important to note that anxiety and depression fell from higher-than-normal levels of anxiety and depression that probably rose in the lead up to the lockdown. Currently, the group is still reporting much higher rates than other age groups.
This has significant policy implications. If lockdowns and social isolation continue to be the main strategy for disease control, we need to take into account that young people face more total loneliness, depression, and anxiety than other age groups. They have also been less happy and less satisfied with their lives. This is perhaps unsurprising given they have faced the greatest upheaval over the past year, with disruptions to education, challenges in securing and maintaining employment, and unstable accommodation.
Young people have also been blamed for driving the spread of COVID-19. This is despite the fact that some of their compliance behaviours are in fact better than other age groups.
As we are forced back inside our homes, we should consider how to help this group that is already vulnerable to psychological difficulties. Young people need ways to interact or gain mental health support, even if they do so online or in socially distant environments. They also need support, stability and understanding.
If we don’t consider these actions, the government may have to manage poorer compliance from young people. Our research suggests that confidence in the government is the most significant predictor of compliance. Young people are already less confident in the government than other age groups, and with decreasing levels of wellbeing that are likely to ensue as we isolate further, they are more likely to ignore COVID-19 guidelines. Helping them manage their mental health is important both for their wellbeing and for disease control overall.
Accounting for inequality
Despite the attempts of leaders to create a sense of unity and togetherness during the pandemic, the truth is we are not all living the same reality. Such rhetoric does not change the experiences of vulnerable groups who entered the pandemic at a disadvantage and have continued to suffer the greatest consequences of the lockdown.
Our research has shown that people from low socioeconomic backgrounds have been disproportionately hurt by restrictions; that people from ethnic minority groups have faced more challenges than white ethnicities; and that the mental health of young adults has been hit particularly hard. Individuals who fall into two or more of these groups need to be most carefully considered for support.
While informed, broad-sweeping measures are required to tackle a national health crisis, the inequalities faced by so many in the UK need to be considered more carefully so that further harm is prevented and government expectations are appropriate and realistic for everyone. Effective control measures are sensitive ones that take into account the individual experiences of those who follow them.
The government would serve its population well if it showed greater appreciation for the struggles of people from poorer socioeconomic backgrounds. When lockdowns are implemented, it is important to realise just how much people with low SEP are affected. Slow, moderate, and unspecific attempts to alleviate economies by geographical region rather than by focusing on the most vulnerable will likely have little impact on these inequalities.
Any future measures to stop the spread of the virus must ambitiously focus on how to prevent people from moving from a position of precarious financial strain to further ruin and to improve the mental health of ethnic minority groups and young people. This is essential for future waves of this pandemic and potential future health emergencies.
Prioritising these groups will lead to greater compliance, less economic hardship for individuals and society as a whole, and the slowing of the spread of COVID-19. In contrast, unspecific, insensitive and universal rhetoric or restrictions will harm everyone’s efforts to end this pandemic.

For you: more from our Insights series:
-
The way we use data is a life or death matter – from the refugee crisis to COVID-19
-
Robots were dreamt up 100 years ago – why haven’t our fears about them changed since?
-
‘We will not forget our colleagues who have died’: two doctors on the frontline of the second wave
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter.
![]()
Daisy Fancourt receives funding from the Nuffield Foundation, Wellcome and UK Research and Innovation.
Alexandra Bradbury does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.










