Dragana Gordic/Shutterstock
As the days get shorter and the weather colder in the northern hemisphere, health officials have warned of a perfect storm of infectious respiratory diseases over the winter months.
Outbreaks of seasonal diseases like influenza and respiratory syncytial virus (RSV) are already putting pressure on the overburdened NHS. If surges of these illnesses collide with another large COVID wave, we could be facing a public health disaster. Some have called this threat a “tripledemic”.
But how can we realistically expect the winter to play out? To try to answer this question, we can look at the recent and current trends of some of the most common winter infections in the UK.
Read more:
Omicron BQ.1 and BQ.1.1 – an expert answers three key questions about these new COVID variants
1. COVID-19
Let’s start with the most obvious one, SARS-CoV-2 (the virus that causes COVID-19). The UK has so far been through multiple COVID waves, fuelled by a combination of behavioural changes, emerging variants and waning immunity.
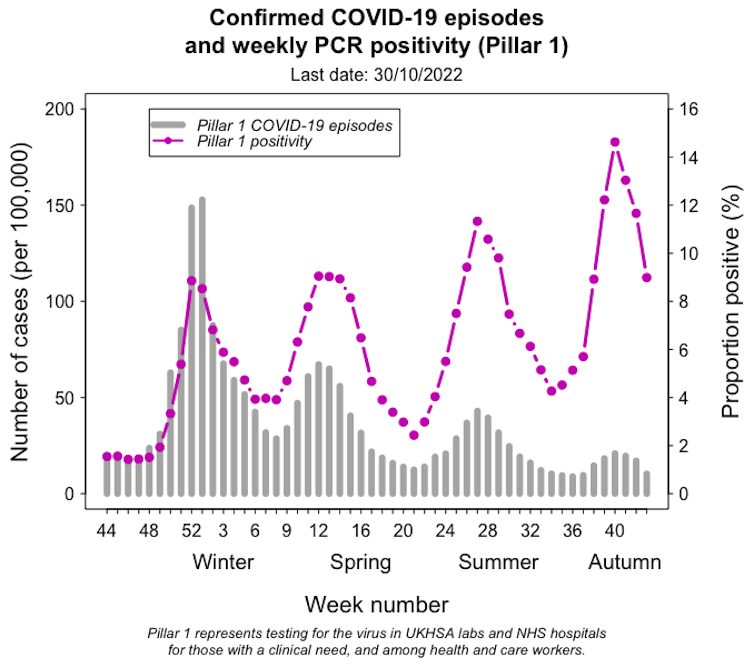
Adam Kleczkowski/UKHSA, Author provided
In contrast to the large epidemic last winter, more recent waves have been relatively small. And despite initial concerns about a significant winter surge this year, the number of COVID cases is currently decreasing. But the pandemic isn’t over yet, and what will happen next is highly uncertain.
So far, there’s mixed evidence as to whether COVID is worse in cold weather. But during winter, people tend to stay indoors more and reduce ventilation, giving viruses more opportunity to spread.
In an optimistic scenario, small-scale outbreaks might continue into the winter as COVID becomes “endemic”.
Previous COVID waves have largely been driven by single dominant variants – alpha and delta in 2020-21 and omicron in 2021-22. This time, the many “descendants” of omicron are multiplying worldwide, and the current spread is instead caused by a mixture of variants peaking in different countries at different times.
But it is possible that if a highly transmissible variant emerges this winter, it might cause another large wave of infections.
2. Influenza
Seasonal influenza is a respiratory infection caused by four types of viruses, two of which (A and B) are common and can cause severe illness, hospitalisation and death, particularly in vulnerable people.
Flu is highly seasonal in climates like in the UK, partly because people spend more time indoors. The virus itself also appears to favour low temperatures and low humidity.
Not unlike COVID, factors including waning immunity and the evolution of influenza viruses also drive repeated outbreaks.
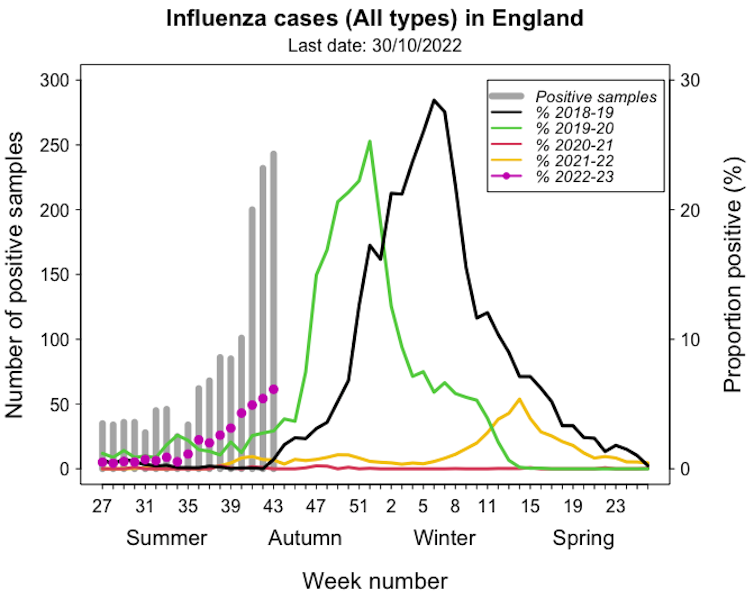
Adam Kleczkowski/UKHSA, Author provided
Flu seasons usually start in November, with cases peaking from December to March. In some years, the outbreaks are particularly severe, as in the UK in 2018.
Flu responded the same way COVID did to non-pharmaceutical interventions, including lockdown restrictions and mask-wearing. The number of cases in the 2020-21 winter was very low. It came back the following season later in the year, but was still limited.
There is concern that the long period during which our bodies were not exposed to the flu might have created an “immunity gap” making us particularly vulnerable this year.
Australia saw the worst seasonal flu outbreak in five years during its recent winter, coinciding with a large COVID surge. While it’s still early to see what the 2022-23 winter will bring in the northern hemisphere, the current outbreak in England is early and large compared with pre-pandemic years.
3. RSV
RSV is a common winter virus which usually causes mild coughs and colds but occasionally results in serious infections like bronchiolitis and pneumonia, particularly in young children.
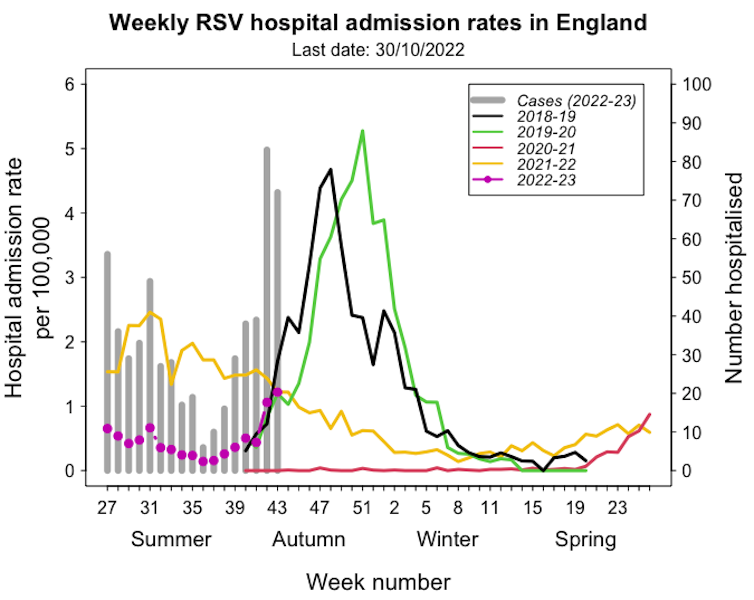
Adam Kleczkowski/UKHSA, Author provided
In pre-pandemic years it followed a seasonal pattern, with most cases occurring in early winter. After a hiatus in 2020-21, many cases were registered out of season in the summer of 2021. This unusual pattern is again suspected to result from a loss of immunity.
The seasonal pattern seems to be returning, but this autumn has already seen high hospitalisation numbers.
4. Common cold viruses
Common colds are caused by a variety of pathogens, including rhinoviruses, enteroviruses, and other coronaviruses.
Like flu, the onset of the more benign coronaviruses generally occurs in November, with the peak between January and March. Rhinoviruses and enteroviruses tend to peak in autumn rather than in winter.
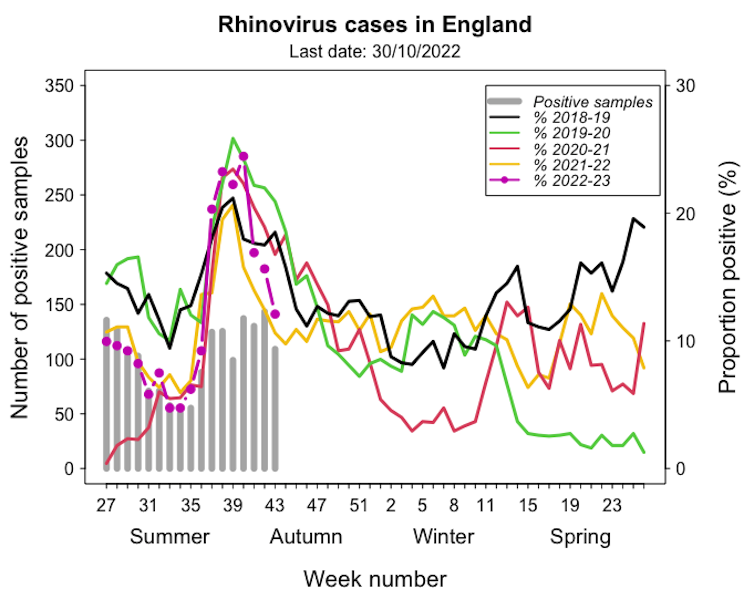
Adam Kleczkowski/UKHSA, Author provided
The 2021-22 rhinovirus season was similar to pre-pandemic trends, but we’re seeing higher numbers so far this year. The infection is usually mild, and most people quickly recover, but severe cases in vulnerable people can add to the pressure on hospitals.
Read more:
Summer colds: this may explain why so many have suffered them this year
Protecting ourselves
This winter, the UK will probably face high pressure from respiratory viruses. Cases of seasonal diseases are possibly higher due to the lack of exposure during the lockdowns. In addition, some research suggests COVID infections might affect people’s immunity, putting them at higher risk of infection with other viruses.
To reduce the spread of respiratory viruses, we can continue with measures like ventilation, mask-wearing and hand-washing.
We can also strengthen our immune systems, for example with proper nutrition and exercise.
And although we don’t have vaccines available for RSV or common cold viruses, COVID and flu vaccines are an important tool to prevent severe illness this winter.
![]()
Adam Kleczkowski receives funding from the UKRI and the Scottish Government.











