Yurchanka Siarhei/Shutterstock
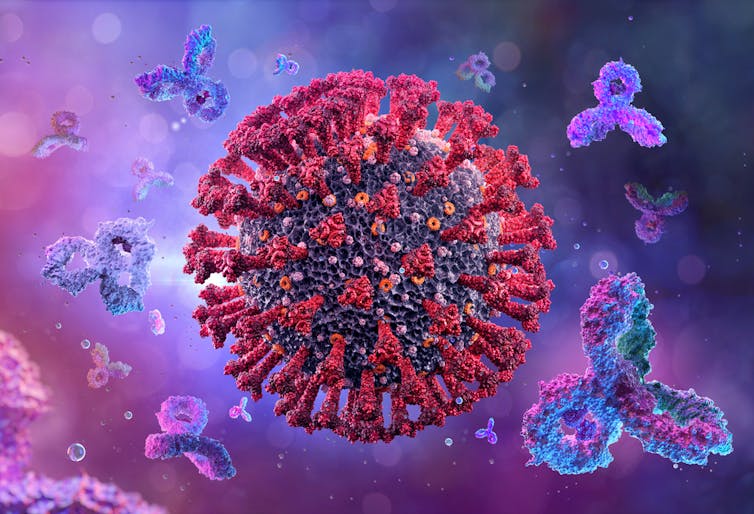
With the highly mutated omicron variant spreading rapidly, people want to know if immunity from vaccination or a prior infection will be enough to protect them against getting infected or developing severe disease.
If prior immunity does provide sufficient protection, then precautionary measures to slow omicron’s spread, together with vaccinating and boosting people, should prevent intolerable strain on healthcare systems. But if not, then increased social restrictions are inevitable as the variant spreads around the world and potentially replaces delta, which is currently the dominant variant.
Early studies – all of which are still preprints, so yet to be formally reviewed by other scientists – suggest that omicron is handled less well by existing immunity. But research also suggests that giving a third booster vaccine dose may provide protection. So, the bad news isn’t as bad as it could be, but the good news also needs to be treated with caution. Here’s why.
More to immunity than antibodies
Inevitably, early reports have focused on the most quickly accessible data, which is the amount of antibodies people have in their blood that are capable of neutralising the new variant.
Overall, the data consistently suggest that omicron can escape these neutralising antibodies to some extent: the reduction in neutralisation in double-vaccinated people is somewhere between 10- to 20-fold to 40-fold compared to delta. That said, in people who had received two vaccinations and had also been infected, the level of neutralisation of omicron was higher.
This may seem alarming. But it’s not the whole story. In previous studies that have looked at earlier forms of the virus, levels of neutralising antibodies have correlated well with levels of protection – greater neutralising activity equating to better protection.
Corona Borealis Studio/Shutterstock
But lower levels of neutralising antibodies doesn’t necessarily mean people are completely exposed. Past studies have also found that many people with low levels of antibodies do still appear to be sufficiently protected, particularly against severe disease, even with the newer variants like delta. We may find that the same applies with omicron.
This is most likely because neutralising antibodies that attack and nullify the virus are just part of the immune response. There are also binding antibodies, which attach to the virus or to infected cells to flag them to other immune cells for destruction, and T cells and memory B cells, which can attack the virus directly and produce more antibodies to fight it.
Even in the initial absence of antibodies that can neutralise the virus, these mechanisms may also provide a level of protection against infection or symptomatic disease. This may still be sufficient to reduce the likelihood of omicron causing severe disease and limit its impact on health systems.
A boost of good news?
Two of the recent reports also strongly suggest that a third booster dose of a COVID vaccine dramatically increases levels of neutralising antibodies against the widespread delta variant and that this would also increase neutralisation of the omicron variant.
One of these (a press release from Pfizer) suggests that a booster can provide quite a marked increase in neutralisation of omicron, although this only included a summary of the results and not the full dataset.
A closer examination of what data is available in these studies reveals that reduced neutralisation of omicron can be extremely variable (which is why it would be helpful to see Pfizer’s results in full). While some vaccinated or previously infected people are good at neutralising omicron, some have almost no neutralising antibodies, even after a booster dose.
So are these people still likely to be protected against infection or severe disease? It’s hard to say. As discussed above, we don’t know the extent to which the immune system’s other mechanisms can provide protection.
However, we do know these other immune mechanisms target different parts of the coronavirus to neutralising antibodies. And while the part of the virus that neutralising antibodies target – the spike protein – is heavily mutated in omicron, the bits these other mechanisms focus on aren’t so badly affected.
We can hope that people with low levels of neutralising antibodies, even after a booster, will therefore be protected by these other immune defences remaining largely undiminished. This, though, is not a given, and we need further studies to measure real-life protection.
Optimism rather than confidence
Overall, then, what we know so far is that vaccination or prior infection should provide some protection against omicron, and that for most people protection should be increased by a booster vaccine dose.
But the crucial message from these early studies is that we still need a lot more information to assess the national and global impact of the rapid spread of this new variant. We need more and larger studies on neutralising antibodies after different combinations of vaccines and previous infections.
We also need studies of the ability of other protective mechanisms (T cells, binding antibodies) to control infections and disease caused by omicron. And we need to know how much these mechanisms are also boosted by a third vaccine dose.
And above all, we need large, real-time studies of levels of infection and disease attributable to omicron to allow rapid, rational public health decisions to be made. Research groups around the world are addressing all these areas and, in the near future, we can expect their reports to make the situation clearer.
![]()
The authors do not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.











