The most powerful tool for combating COVID is not a drug or a vaccine, but a method. A randomised trial is the best way to discover what works and what doesn’t. This method underlies much of the progress in modern medicine, including the development of effective COVID vaccines. However, developing highly effective vaccines is not enough. We also need people to take them. Again, randomised trials should be our guide.
Early in the pandemic, drugs such as hydroxychloroquine were championed as effective treatments for COVID. Many, including prominent politicians, questioned the need for traditional randomised controlled trials (RCTs) as the drugs had been previously used to treat other illnesses and were deemed safe. It was thought that RCTs could unnecessarily delay patients receiving potentially life-saving treatments.
In an RCT, patients are randomly allocated to receive the drug being tested or to receive a placebo (or usual care). This way we can determine with a high degree of certainty whether the drugs reduce the severity of illness and save lives.
RCTs, such as the Recovery, the world’s largest clinical trial, showed that many candidate treatments for COVID, including hydroxychloroquine, did not work, while other drugs, including the low-cost dexamethasone, can save lives. These findings from RCTs were quickly put into practice and have helped save over a million lives.
While RCTs have told us which drugs work and which don’t, their use in tackling more human aspects of the pandemic has been much more limited. A recent estimate suggested that while there are more than 2,000 COVID-related drug trials in progress, there are only 17 RCTs of behavioural interventions to control the pandemic.
In countries such as the UK, which has now vaccinated more than 75% of its adult population, the delta variant is still spreading, with more than 200,000 cases in the past week. Of particular concern in the UK are the low vaccine uptake rates in younger age groups and among black adults, where reported hesitancy is five times greater than white adults.
Policies to promote vaccine uptake are now seen as key to managing COVID. Countries are adopting a number of different incentives. Vaccine lotteries are being offered in the US, Canada, Poland and Hong Kong, while cash payments are being used in Serbia and the US. In the UK, fast food (dubbed “kebabs for jabs”) is being offered.
In Africa, the key problem is vaccine supply, with less than 2% vaccinated. Yet those thinking one step ahead, such as development economist Rabah Arezki, are advocating that cash transfers become integral to vaccine rollout in Africa and other low and middle-income countries to ensure the highest global vaccine coverage.
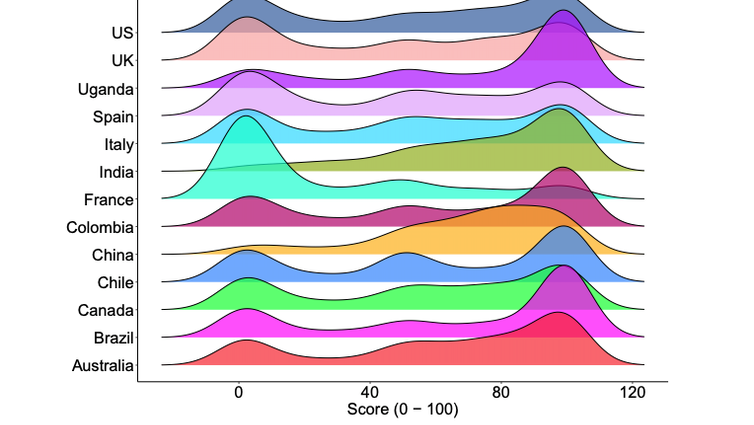
Beyond incentives, countries are also considering penalties for the unvaccinated to further promote uptake. Italy and France require evidence of vaccination to engage in a range of activities, including going to restaurants, theatres and sporting venues. This has brought tens of thousands of people onto the streets to demonstrate against such measures. As the graphic below shows, opinion (x-axis) is skewed toward making COVID vaccination mandatory, but there is evidence of polarised attitudes in many countries.
Extent to which people agree that government should make COVID vaccination mandatory (x-axis)
Figure adapted from preprint: https://www.medrxiv.org/content/10.1101/2021.01.31.21250866v1.full.pdf
While incentives are often easier to implement, as they do not normally induce such opposition, it is likely that a combination of incentives and penalties will be needed to raise vaccination rates to a high enough level to effectively combat COVID.
Incentives haven’t been put to the test
Unlike the development of COVID vaccines, which were only made available to the public after a careful evaluation of RCT evidence, policies to promote vaccine uptake through incentives or penalties appear to be introduced without any formal testing to evaluate their effectiveness.
Take the Ohio vaccine lottery, introduced in May, which involved giving cash prizes of up to a million dollars for those getting vaccinated. There have now been at least four studies trying to retrospectively estimate its effect on vaccine uptake, two of which have found that the lottery had no effect and two which have found it promoted uptake. While it’s tempting to repeat Winston Churchill’s quip that “if you put two economists in a room, you get two opinions”, it illustrates the difficulties of conducting policy evaluation without the benefit of being able to randomise.
Are randomised vaccine incentives experiments really possible? One way is to take advantage of the multitude of incentives across the US, making it the world’s vaccine-incentive policy laboratory. All one needs to do is add randomisation to see what works.
We recently took this approach by randomly allocating just over 1,600 unvaccinated Americans to one of three brief video messages, including information that those getting vaccinated might be eligible for a cash payment or a vaccine lottery. Our results, which we uploaded to the medRxiv preprint server, show that cash incentives, but not vaccine lotteries, are likely to promote vaccine uptake. An extra 5% of those seeing the video about cash incentives clicked through to get information on where they could get vaccinated.
Beyond understanding the overall effects of incentives and penalties, it is important to look at what works best in key sub-populations. This particularly includes those populations with low vaccine uptake and those most likely to spread COVID in the community.
When it comes to incentives to promote vaccine uptake, evidence from RCTs is the sieve that separates good policies from bad ones.
![]()
Philip Clarke receives funding from the Medical Research Council, the COVID-19 Oxford Vaccine Trial and the NIHR Oxford Biomedical Research Centre.
Laurence Roope receives funding from the Economic and Social Research Council, the Medical Research Council, the COVID-19 Oxford Vaccine Trial and the NIHR Oxford Biomedical Research Centre.
Raymond Duch does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.