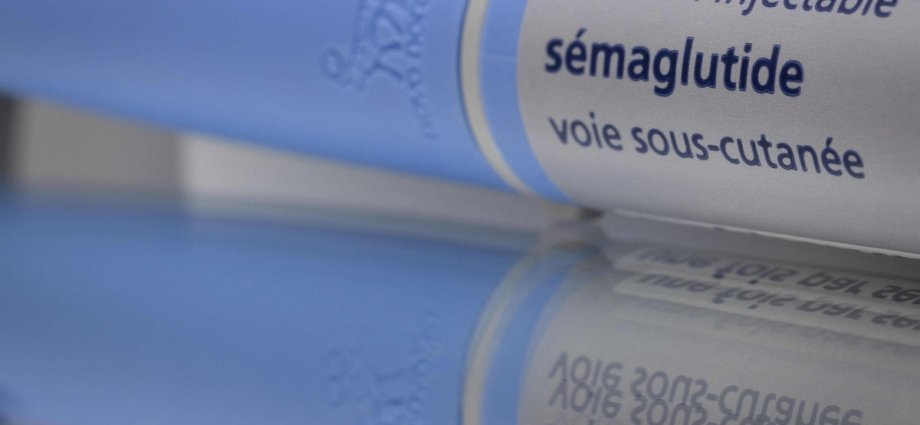
Drugs like semaglutide, the active ingredient of Ozempic and Wegovy, are more effective in treating type 2 diabetes than conventional treatments, a comprehensive new comparative study finds.
About one in nine adults globally has diabetes, with over 90 per cent of the cases living with type 2 diabetes and requiring effective management of their blood sugar levels.
Managing diabetes involves regulating a variety of factors, including patient lifestyle, co-morbidities, and the potential side effects of medications.
Currently, the drug Metformin is widely given as the first-line of treatment due to proven safety, its effectiveness and affordability.
However, nearly two-thirds of those on Metformin are often prescribed additional treatment over time to maintain their blood glucose within recommended levels.
Now, a new study has assessed various glucose-lowering treatments among adults with type 2 diabetes.
-made-by-Danish-pharmaceutical-company-Novo-Nordisk.jpeg)
The latest research analysed data from over 8,000 participants from diverse backgrounds, encompassing a range of ages, genders, and socioeconomic statuses, reflecting the true demographics of individuals commonly diagnosed with type 2 diabetes mellitus.
Scientists hope the timely findings of the study could serve as a vital resource for clinicians seeking to optimise treatment plans for their patients.
Researchers found that some treatments lead to more substantial improvements in glycemic control compared to others.
Particular drugs, such as GLP-1 receptor agonists, the class to which Ozempic and Wegovy belong, may outperform traditional therapies in various clinical scenarios, researchers found.
“GLP-1RAs were most effective for glycemic control,” scientists wrote in the study published in the Journal of General Internal Medicine.
Sodium-glucose cotransporter-2 inhibitors (SGLT-2is), a class of drugs that block glucose reabsorption in the kidneys, were also found to be effective with a lower risk of heart failure hospitalisation among those taking them.
Another class of drugs called sulfonylureas, which work by stimulating the pancreas to release more insulin, was found to work reasonably well for lowering glucose but carried a higher risk of low blood sugar episodes.
Drugs that trigger insulin release after meals, called DPP-4 inhibitors (DPP-4is), were found to be the least effective among the four at maintaining glucose levels, without offering any unique benefits.
Citing a limitation of the study, scientists said the study cohort was restricted to privately insured US individuals, which may limit the generalisability of the findings to other populations.
However, they say the findings point to an evolving paradigm in diabetes care, advocating for newer clinical strategies that not only control blood glucose levels in diabetes patients but also confer cardiovascular and renal benefits.