The UK is facing a cancer care “disaster” as NHS staff cuts mean patients can’t get the potentially life-saving treatment they need fast enough, senior doctors have warned.
More people than ever are surviving cancer, and death rates have decreased by 22 per cent in the past 50 years, but diagnoses ballooned to more than 354,820 in 2023, compared to 327,174 before the pandemic, as early diagnosis improves and treatment options have increased.
But as more people than ever are being diagnosed, fewer are being treated within the government’s 62-day target for urgent referrals, with 100,000 waiting longer in 2025, analysis of NHS data by Cancer Research UK for The Independent shows.
On Wednesday, the government will unveil its 10-year plan aimed at turning around cancer services in England, which will include a pledge to hit all NHS cancer waiting time targets by 2029, and give more patients access to cutting-edge treatments, such as robot-assisted surgery and genomic testing.
However, experts have warned that overstretched services are already struggling to deliver treatments and train enough staff in the new techniques.
The NHS aims to have 85 per cent of patients treated within 62 days; however, the most recent data shows just 70 per cent of cancer patients were treated within this time last year. Cancer Research said that even if the NHS had met this target, 51,100 people would still not have started treatment on time.
Doctors say the delays mean some patients’ cancer has progressed to later stages by the time they are seen, which means they often need additional or more invasive treatments, piling further pressure on services.

The new details on the flagship cancer plan come after the Royal College of Radiologists (RCR) has warned that the NHS faces a shortfall of nearly 2,000 doctors to meet demand, which will rise to 3,646 by 2029. It says the issue is being exacerbated by hospital budget cuts, which have forced a pause on hiring extra staff.
Dr Nicky Thorp, the RCR’s vice-president for clinical oncology, said: “I think that’s a potential disaster because that’s also creating bottlenecks we have. It’s not that we don’t have people to fill posts. We do have people to fill posts, but they are unable to get jobs.”
The warning comes as diagnosis figures are rising for the most common cancers in England – prostate, breast, lung, and bowel. The most recent data, published in 2025, which details diagnoses in 2023, show:
- More than 50,500 cases of breast cancer were diagnosed in 2023 – 2,264 were at stage 4. This compared to 45,282 with 2,166 at stage 4 in 2013
- There were 58,137 prostate cancer diagnoses in 2023, up from 40,372 in 2013
- Lung cancer diagnoses have risen from 37,805 in 2013, to 42,082 in 2023
- Bowel cancer diagnoses increased from 34,528 to 40,907 over the same period
At the same time, deaths are falling as more people survive or are able to live with cancer, with figures showing 138,578 deaths in 2023, a rate of 240.2 per 100,000 people, compared to a rate of 284 in 2013.

Meanwhile, separate waiting list figures for England from April 2025 to November 2025, the most recent month available, show that the government is failing to hit its target of 75 per cent of patients being diagnosed within 28 days, with 73 per cent of people getting their results on time. Meanwhile, 91 per cent of people are treated within 31 days of a treatment plan being made – behind the 96 per cent target.
Under the 10-year plan, the government has promised that all patients who need it will have access to genomic tests, which can analyse cancer DNA to help doctors personalise treatments, which could be more effective.
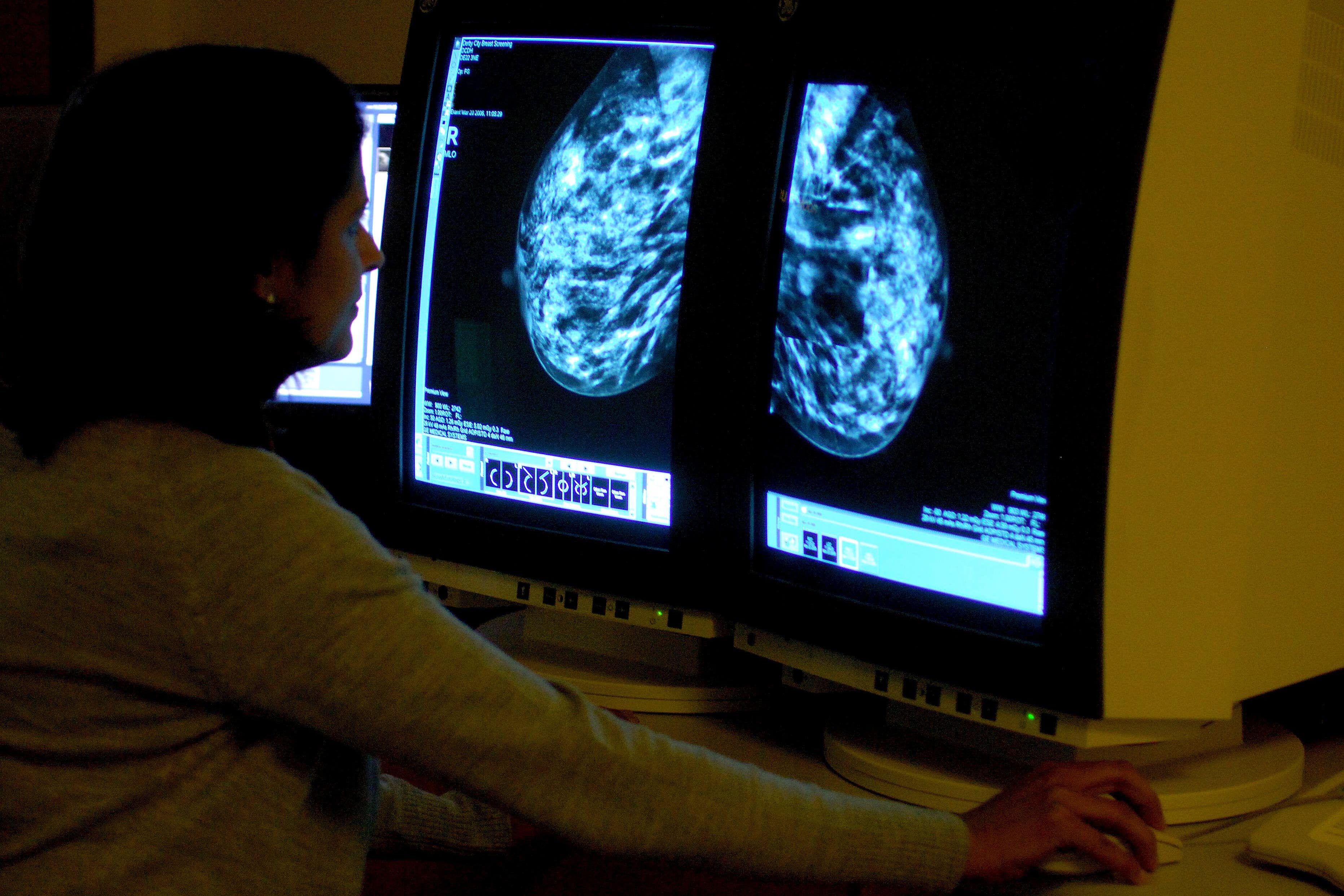
Currently, 13,400 of the 17,000 patients waiting longer than 62 days for treatment were waiting for a diagnostic test, such as a HER2 test, used to determine the best treatment for aggressive breast cancer.
Dr Andrew Wardley, president of the Association of Cancer Physicians, who works at hospitals in Manchester, said some patients were waiting up to three weeks for the “basic test”.
He said: “We’ve got postcode prescribing now in terms of our ability to provide the right staff to treat the patient. There aren’t enough people, everyone’s overworked, demoralised, and concerned about patient safety. Patients are having their treatments delayed, they’re not getting treated on time, and everything else you can think about is just about gone wrong.
He added: “Pathology [testing] services are in a state where you’re not getting the results to make treatment decisions in time, in a good time. Fairly basic test results like HER2 are taking up to three weeks in some places, which is far too long to keep patients in that pressing kind of circumstance.”

Dr Wardley warned that recruitment freezes were impacting oncology services and said staffing shortages were affecting even the largest NHS trusts, with some patients forced to seek private care.
Breast cancer is the most commonly diagnosed cancer for women in England, with more than 50,000 cases diagnosed a year. But despite the rising number of diagnoses, screening rates for women over 50 have fallen from 74 per cent in 2019 to 70 per cent in 2024.
Breast reconstruction surgeon Angela Waters, who works at University Hospitals Birmingham, told The Independent that surgeons were “overwhelmed” with the demand, and her hospital has had to restrict referrals and is now only accepting local patients.
“We haven’t got enough surgeons who can do it, so those of us who are doing it are overwhelmed with work at the moment, and some areas of the country are well served, and others aren’t really offered it at all… it’s just completely unfair and not a situation we should be in, really,” she said.
“It is really awful, because… the ones who didn’t have breast cancer, but were at high risk while they’re waiting, they get breast cancer. It is really awful. It’s incredibly distressing for anybody who’s on that rating list.”
Angela Baker, chair of the Society of Radiographers Radiotherapy Advisory Group, said that while advances in technology, such as stereotactic body radiotherapy (SRT), which targets tumours from multiple directions, have sped up treatment, services need the funding and staff to deliver them.
“So it’s a bit of a catch-22 situation. You need staff to train staff,” she said.
Dr Baker also said that services were increasingly seeing patients with later-stage cancer due to delays, meaning more patients had to be referred for additional treatments.
“We’re all struggling a bit, I think, from lack of resources… what that means to be able to deliver safe treatment… we need to extend clinical (hours), but we can’t do that as we don’t have the staff.”
Dr Thorp agreed that NHS cost savings were hampering treatment times.
She said, “Increasingly, hospitals are being told you cannot recruit. You’ve got to save, you’ve got to save money. There’s no more money… Doctors, nurses, scientists, really, lots of, you know, all the people that we need to treat our patients.”
“I really acknowledge that there is not infinite money in the system, but one also has to acknowledge that if you really want to improve things, you cannot say, we want to improve things, and then not do anything about it. So the recruitment freezes, I think, are a disaster. They’re a disaster for all patients.”
A Department of Health and Social Care spokesperson said: “There are now a record number of doctors working in the NHS in England – over 6,200 more than last year – and since this government came to office, we have recruited an additional 2,900 GPs. We are rebuilding our NHS so it is there for all cancer patients when they need it.”
NHS England has been approached for comment.











