Health bosses are aiming to tackle “poor care” faced by many children and young people living with sickle cell disease when they move to adult healthcare providers.
NHS Race and Health Observatory, an independent body which examines inequality in healthcare, will work with the Sickle Cell Society charity with the aim of improving the transition for patients into adult care.
It is estimated around 300 babies are born with sickle cell disease each year in the UK and young people with the illness “often experience poor care in non-specialist settings” when moving to adult care, the body said.
Professor Habib Naqvi, chief executive of NHS Race and Health Observatory, said: “By improving trust within the care pathway we can tackle gaps in care, learn from successful outcomes in transition from other disorders and initiatives, and ensure excellent patient-centred care is provided.
“It’s vital that patients with sickle cell disorder, and other chronic conditions, receive optimal transition from paediatric to adult services from specialists and general hospital staff at, what is, a vulnerable stage in life.
“This programme will help to ensure young patients are well-supported and their pain is managed effectively during the process to avoid lasting harmful consequences.”
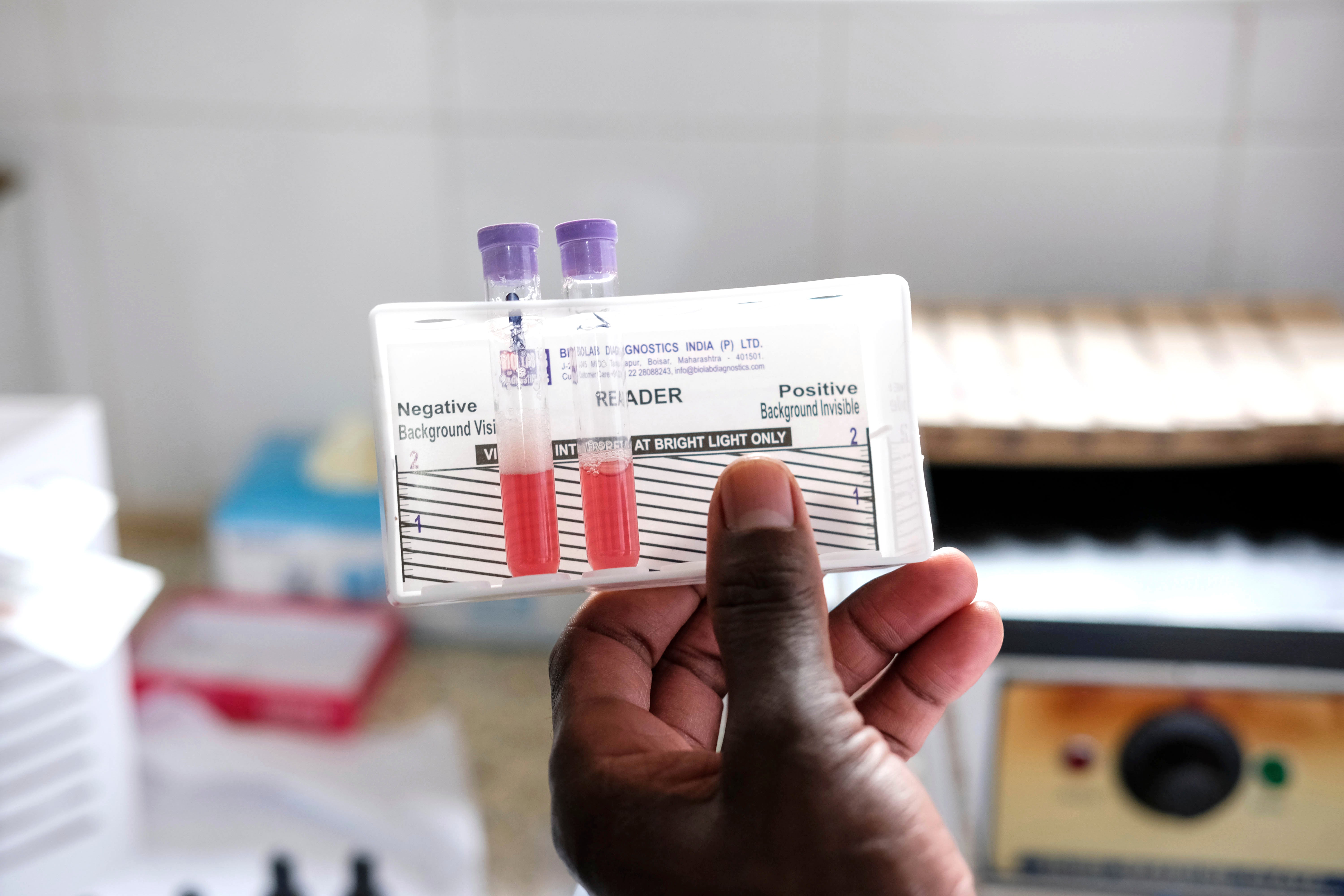
Sickle cell disease is an inherited long-term and potentially life-threatening condition which is more common among Black people. It affects about 15,000 people in England.
It causes debilitating pain and multiple problems such as severe infections, strokes, chronic fatigue, delayed growth, and progressive tissue and organ damage.
Patients and campaigners have long decried a lack of awareness around the illness in the UK, as well as issues with substandard care for those affected.
A recent report highlighted a chronic shortage of specialist sickle cell nurses is putting lives at risk.
A 2021 all-party parliamentary group (APPG) report on sickle cell and thalassaemia found “serious care failings” in acute services and evidence of attitudes underpinned by racism.
This new research will capture young people’s experiences and views on treatment plans that are “often ignored” to ensure they feel supported and empowered to deal with the condition as adults.

It will also focus on addressing the long-term needs of young patients, particularly from the ages of 12 and 13 up to the age of 18.
This will include evaluating new and existing optimal apps and online resources, effective policy initiatives, and anecdotal feedback from face-to-face interactions. It will be backed by engagement with health bodies, red cell specialists, patients, their families and carers during visits to hospital wards and A&E admissions.
The move comes after the parents of a 22-year-old sickle cell patient, Darnell Smith, who died after hospital failings, told The Independent the NHS is letting sickle cell patients down.
John James, chief executive of the Sickle Cell Society, hailed this move as “a huge opportunity to transform the experiences of young people with sickle cell disease”.
“The transition from paediatric to adult care can be an overwhelming process, and many patients face challenges that significantly impact their health and well-being,” he said.
NHS Race and Health Observatory was launched in 2020 and is an independent body hosted by the NHS Confederation and supported by NHS England.
It provides evidenced recommendations and practical solutions regarding inequalities affecting ethnic minority patients, communities and the healthcare workforce.
Professor Bola Owolabi, NHS director for healthcare inequalities, said: “Sickle cell disease can have a devastating impact on people’s lives which is why the NHS has worked hard to make life-changing treatment available as part of our wider drive to improve the quality and experience of care for sickle cell patients.
“This includes securing the latest cutting-edge therapies, promoting a scheme to help with prescription costs, piloting 24/7 expert clinics for patients in sickle cell crisis which allow them to bypass A&E to receive pain relief, digital care plans so patients don’t need to repeat their stories, plus cutting-edge blood group genotyping to reduce the risk of adverse reactions to blood transfusions.”











