Several labs will work with federal health authorities to develop a test for avian influenza, as the number of human cases rise across the country.
The Utah-based ARUP Laboratories said Friday that it was selected by the Centers for Disease Control and Prevention (CDC) as one of five lab partners, along with Quest Diagnostics, Labcorp, Aegis Sciences, and Ginkgo Bioworks.
The CDC decision ensures that labs can work with the agency, responding to outbreaks and testing in real time.
Last week, a person in Missouri was infected with bird flu despite not having any exposure to animals. The state’s health department said the individual recovered from their illness but that a household contact of the patient had become ill with similar symptoms on the same day.
The CDC said that no additional cases had been found, and that the risk of infection among the general public remains low.
“There is no epidemiologic evidence to support person-to-person transmission of H5 at this time,” the agency said.

However, 14 cases of human bird flu have been reported in the US since since April. Of those, four were associated with an exposure to sick dairy cows and nine were related to virus-infected poultry.
Those infected included farmworkers in Colorado, Michigan, and Texas. A dairy worker in Texas was the first instance of cow-to-human transmission. A recent study found the virus in the wastewater of 10 Texas cities, from March through July. Those who were infected experienced mild symptoms and have recovered.
Transmission of the highly contagious avian flu occurs through the infected saliva, mucous, and poop of infect birds, or in the milk, bodily fluids, organs, blood, and respiratory discharge of other animals. Humans are infected when the virus enters the eyes, nose, mouth, or is inhaled. The virus is spread through the air, or when people touch something that is contaminated and then touches a vulnerable part of their body.
Illness in humans can range in severity from no symptoms or mild illness to severe disease that results in death. Symptoms include red eyes, mild flu-like symptoms, pneumonia, fever, cough, sore throat, runny nose, muscle or body aches, fatigue, trouble breathing, and headaches.
One pressing concern is that the virus could mutate further, enabling easier infection among humans, ARUP said.
The CDC currently recommends testing for the virus by public health laboratories using “real-time reverse-transcriptase polymerase-chain-reaction,” or rRT-PCR. Many people may be familiar with PCR tests from the pandemic: molecular tests that have been used to detect Covid. Nose, throat, and other respiratory swabs are analyzed to look for genetic material of the virus.
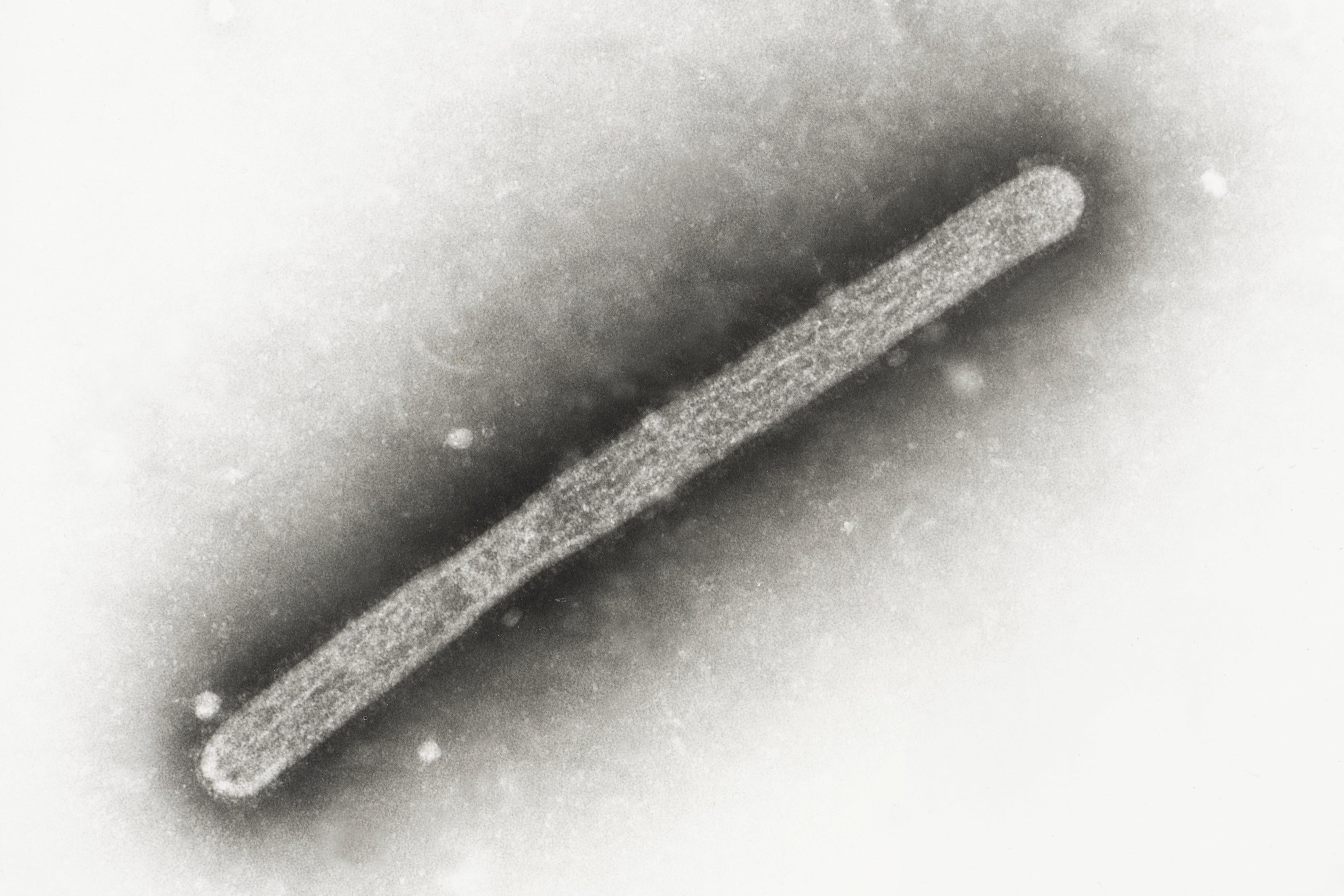
Like Covid, avian flu is caused by an RNA virus, known as Influenza A. These viruses are predominantly spread by birds or pigs.
While DNA is the long molecule that makes up human beings’ unique genetic code, RNA plays a crucial but different role. It helps to carry instructions from DNA molecules to build proteins that help the body run. In existing and commercially available rRT-PCR tests, scientists use tests called molecular assays to determine virus levels.
In August, ARUP Laboratories said it was ready to scale up its testing capacity and had updated the CDC’s test to match the current strain of avian flu, known as H5N1. Should the need for higher volume testing arise, it could use machines.
“Even if bird flu never becomes a huge thing, making a (polymerase chain reaction [PCR]) test is a minimal investment when you consider the huge public health impact it can have,” Dr Benjamin Bradley said.











