A landmark report into the NHS has described the health service as “in serious trouble” as Labour vows to act on its findings. The review by Lord Darzi says honesty is needed if healthcare in the UK is to be improved, highlighting many issues.
The rapid review, completed in nine weeks, diagnoses the problems in the NHS in England and sets out themes for the government to incorporate into a 10-year plan for reforming the health service.
The study argues the NHS is facing rising demand for care as people live longer in ill health, coupled with low productivity in hospitals and poor staff morale.

Speaking at an event in London on Thursday, the prime minister, Sir Keir Starmer, was due to say: “The NHS is at a fork in the road, and we have a choice about how it should meet these rising demands.
“Raise taxes on working people to meet the ever-higher costs of an ageing population – or reform to secure its future.
“We know working people can’t afford to pay more, so it’s reform or die.”
Lord Darzi, a widely respected surgeon and former health minister, argues in his report that the NHS can be fixed.
He said: “Nothing that I have found draws into question the principles of a health service that is taxpayer-funded, free at the point of use, and based on need not ability to pay.”
Here are some key findings from the Darzi report:
The health of the nation has deteriorated
Factors affecting health, such as poor quality housing, low income and insecure employment, “have moved in the wrong direction over the past 15 years”, writes Lord Darzi.
“With the result that the NHS has faced rising demand for healthcare from a society in distress”.
Lord Darzi points out that there has been an increase in multiple long-term conditions. This includes mental health issues, particularly among young people.
This has been worsened by a real-terms cut to the public health grant – given to local authorities by the health department – of 25 per cent.
Spending is poorly distributed
Lord Darzi writes that the NHS budget “is not being spent where it should be”, recommending that more be spent in the community, and less in hospitals.
He notes a positive trend in hospital staffing, with numbers increasing between 2019 and 2023 by 17 per cent. Over the last 15 years, 35 per cent more nurses have joined for adult patients, and 75 per cent more for children.

However, the number of appointments, operations and procedures has not increased at the same pace, pointing to reduced productivity.
“Patients no longer flow through hospitals as they should,” writes Lord Darzi. He says that a lack of funds means hospitals are unable to be productive, while the “dire state” of social care means 13 per cent of NHS beds are occupied by people waiting for support.
This broken system has not reduced the workload for staff, he says, rather it “crushes” their enjoyment of work.
“Instead of putting their time and talents into achieving better outcomes, clinicians’ efforts are wasted on solving process problems, such as ringing around wards desperately trying to find available beds,” he adds
Waiting times have become unsustainable
Waiting times targets are being missed across the board, including for surgery, cancer care, A&E and mental health services. The report says “long waits have become normalised” and “A&E is in an awful state”, with long waits likely to be causing an additional 14,000 more deaths a year, according to the Royal College of Emergency Medicine.
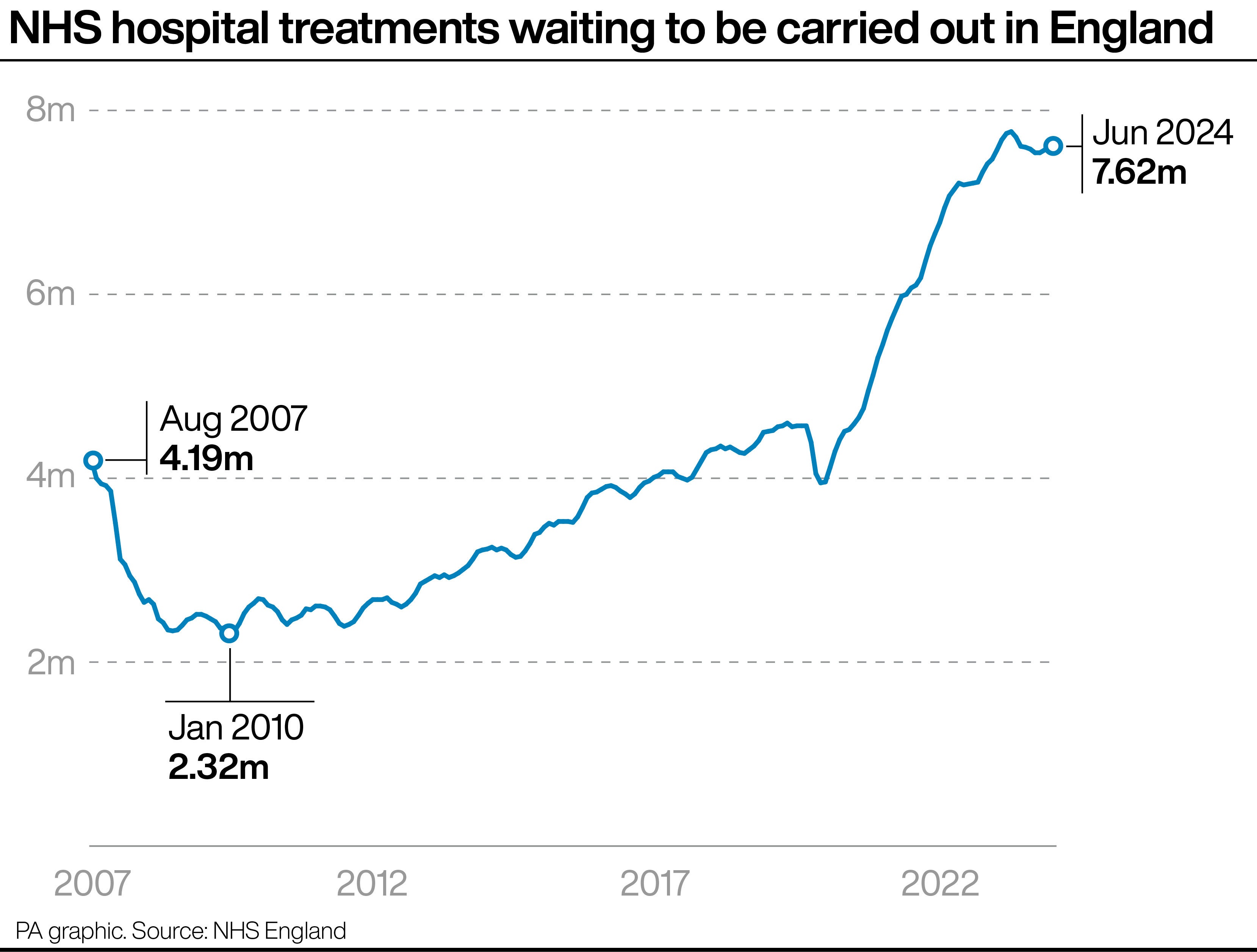
By April 2024, about one million people were waiting for mental health services. The overall NHS waiting list stands at 7.6 million.
“It is inevitable that public trust and confidence will have been damaged by the inability of the NHS to meet the promises of the NHS constitution for the reasons that this report describes,” he writes.
Cancer care has declined
Cancer care still lags behind other countries and cancer death rates are higher than in other countries.
There was “no progress whatsoever” in diagnosing cancer at stage I and II between 2013 and 2021. However, more recent figures show some improvement.
“The 62-day target for referral to first treatment has not been met since 2015 and in May 2024, performance was just 65.8 per cent,” writes Lord Darzi.
“More than 30 per cent of patients are waiting longer than 31 days for radical radiotherapy.”
Austerity in the 2010s hit the NHS hard
Lord Darzi writes that “the 2010s were the most austere decade since the NHS was founded”. He points out that spending grew by only around 1 per cent in real terms across the decade.

He also criticises later Conservative governments for underfunding health services. Lord Darzi says that the 2018 promise to increase spending 3.4 per cent a year was “broken”, with an increase of just under 3 per cent a year from then until now.
Sir Keir said: “The 2010s were a lost decade for our NHS… which left the NHS unable to be there for patients today, and totally unprepared for the challenges and opportunities of tomorrow.”











