A doctor has described the harrowing reality of Britain’s A&E wards as she reveals staff are sometimes forced to give end of life care with patients in corridors on trollies.
Dr Rachel Clarke, a top palliative care doctor, shared the “grim” conditions found in NHS hospitals as she says “Dickensian” conditions are now the norm.
The former journalist who later retrained as a doctor recalled turning up for her shift in the morning to see a “broken” team and ten ambulances queuing outside the hospital with patients.
“You can’t really exaggerate how grim and crisis laden conditions are,” she told the Former Downing Street Director of Communications Andy Coulson on his Crisis What Crisis? podcast.

“You know, we all see the news headlines. I walk into the A&E handover in the morning and I see a team who look absolutely broken from the night shift,
“There are ten ambulances queueing outside each with a patient, some of those patients are dying, they literally can’t even get into the hospital. There are patients in corridors on trollies.
“I might have to have an end of life conversation with a patient on a trolley in a corridor who doesn’t even have a curtain around them. It’s horrific, it’s sort of Dickensian. This is how broken the NHS is at the moment.”
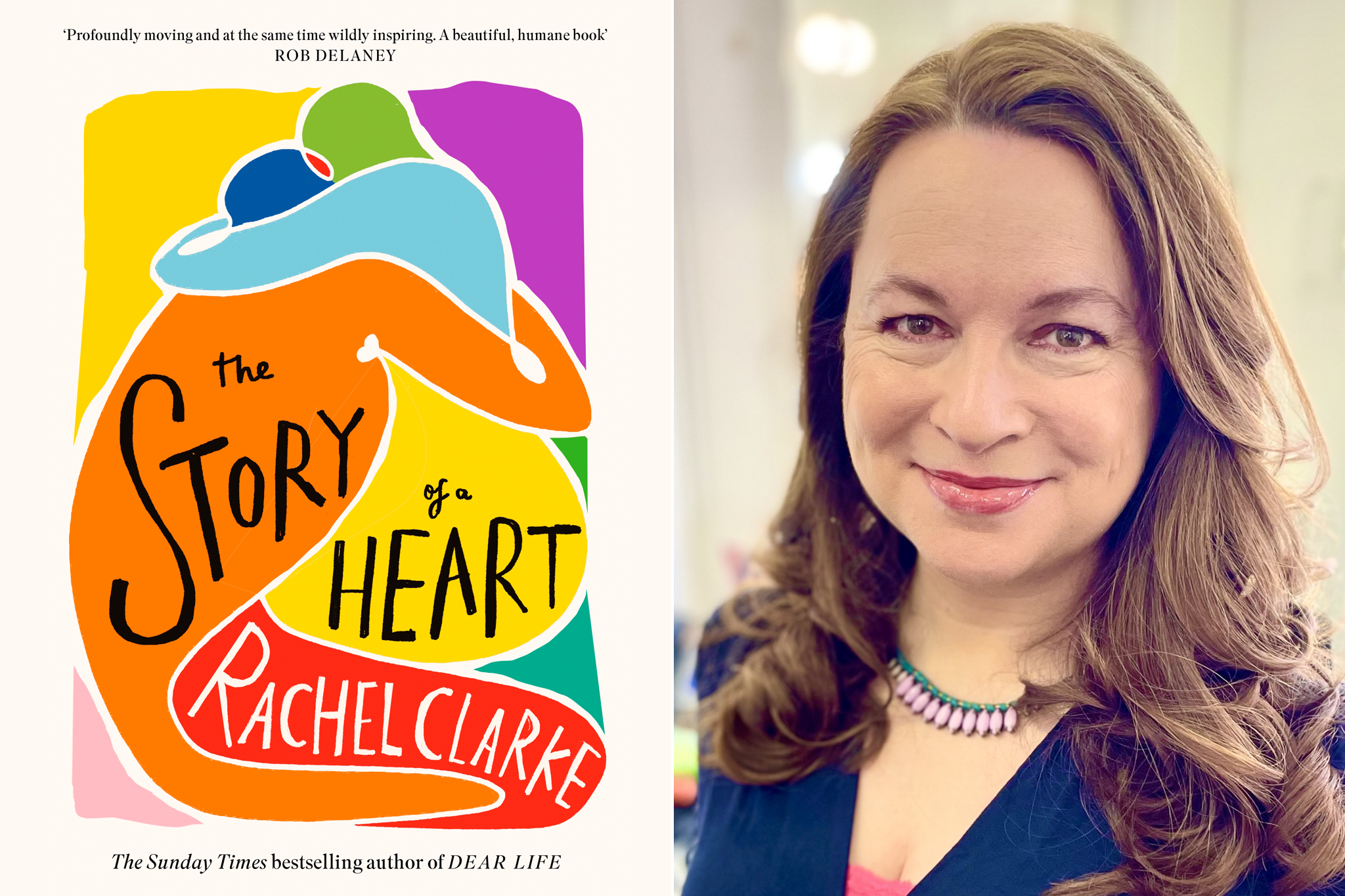
Formerly a current affairs journalist, Dr Clarke re-trained and qualified as a doctor in 2009. Now specialising in end-of-life care, she is the author of Breathtaking , an account of working in the NHS during the Covid-19 pandemic, which was later adapted into a TV show.
Her other works include a memoir about life as a newly qualified medical practitioner, Your Life in My Hands (2017), and Dear Life (2020), which explores death, dying and end-of-life care.
Dr Clarke’s latest book, The Story of a Heart, follows the true story of two families linked after a nine-year-old boy is given the heart of a girl of the same age who suffered catastrophic injuries in a car crash.
Discussing the state of palliative care in the NHS, the doctor continued: “I think if people in Britain – if the public knew that there were people suffering at the end of their life in this way, that was wholly avoidable, that we could fix if we changed the way we are managing the NHS and funding the NHS, they would want to do that immediately. You wouldn’t wish that on your worst enemy, let alone someone you loved.”
She added that crisis conditions on A&E wards are the “norm now and it’s horrendous” as she described staff working in conditions that feel “like fire-fighting”.
‘You really have to be on your best possible game as a doctor, because you have patients who are frightened, who are in extreme suffering, families who are distressed, and you have to go into that crisis situation and try and make a difference, do the best job you can,” she said.
She went on to say she was “delighted” with new Health Secretary Wes Streeting’s statement that the “NHS is broken” and “needed saving”.
“I was really delighted that he said that, because it’s just empty pretence pretending otherwise. That doesn’t help anybody. The NHS is in crisis,” Dr Clarke said.
“It has been for a very long time. And you know, there’s a very simple bottom line here which is a country gets the health service it is willing to pay for.”
A Department of Health and Social Care spokesperson said: “It is unacceptable that patients are waiting so long for care. We have been clear that fixing the NHS will take time, but this government will deliver the investment and reform needed to turn it around.
“We have commissioned Lord Darzi to provide an honest assessment of the state of the health service, and are committed to ensuring all patients, including those at the end of life, receive the standard of care they deserve.
“We are also determined to shift more healthcare out of hospitals and into the community, so patients and their families can access personalised care – where and when they need it.”











