Just when it looked like COVID cases were starting to fall after the high peaks of January, infections are rising once again around the world. The main driver of this latest surge is the more infectious BA.2 sub-lineage of the omicron variant, which has been becoming more common ever since Christmas.
In the UK, increased social mixing and waning vaccine effectiveness – even in those who have had a booster dose – are contributing to this rise. But we’re also seeing huge spikes in areas that had previously kept themselves fairly COVID-free – New Zealand, Hong Kong and South Korea, for example.
Case rates in these places are currently outstripping those seen in many European countries when they were at their worst, despite these newly struggling countries tending to follow rigorous zero COVID policies, with tight border controls and strict internal measures to limit infections. The highly infectious new variant having a bigger effect in places where restrictions are tighter. But why?
Zero cases equals delayed cases
Long before COVID, it was known that non-pharmaceutical control measures – whether within a country or at its border – rarely stop a pandemic spreading. Usually, these things – lockdowns, quarantines and so on – only delay a disease’s spread. However, this may be sufficient to flatten the curve of infections and ease pressure on health services, or to reduce illness and death by delaying most infections until treatments have improved or vaccines become available.
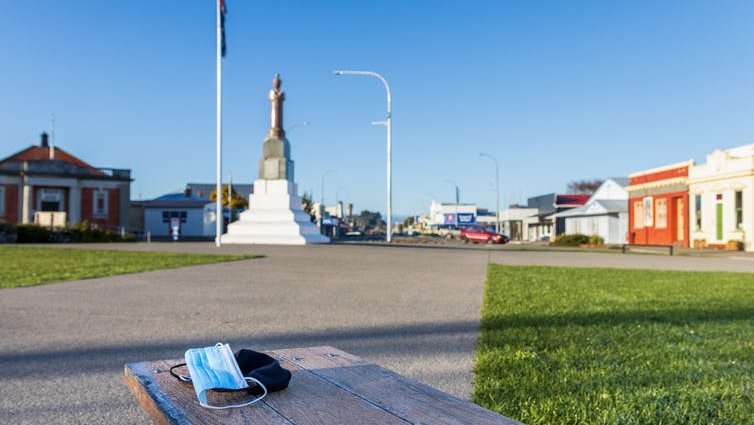
Ross Gordon Henry/Shutterstock
In reality, the most influential disease-control factor is immunity, which can be generated by infection or vaccination. Both are important. As I pointed out last summer, the end of the pandemic in any country will likely depend on the proportion of people who have already had a COVID infection, and not just the proportion vaccinated.
Breakthrough infections in those who are vaccinated will drive their immunity to a higher level, while in the unvaccinated an infection provides a level of protection that would otherwise have been absent. In fact, immunity following an infection now gives rather better protection against being infected in the future than immunity from a booster vaccine, especially once 90 days have passed since being vaccinated.
This helps to explain why some countries are now handling outbreaks better than others. In the UK, despite excellent vaccination coverage, the majority of people have also now caught COVID, and many people have caught COVID more than once. Cases are high for sure, but not as high as in some of these Pacific countries, and rates of death and severe disease are remaining at a relatively low level.
In comparison, countries that followed a zero COVID strategy are now seeing a larger surge in infections and deaths as they open up, even if they have high vaccine coverage. Their lack of prior infections means immunity across the population is lower.
Vaccines still making a difference
But despite the fact that both Hong Kong and New Zealand have both suffered huge rises in viral transmission recently, the impact on public health in the two places has been dramatically different.
New Zealand, with high vaccine coverage and a recent booster programme, is weathering this surge with far fewer deaths so far. Hong Kong has seen many more deaths, with a death rate per million people in the four weeks up to March 18 2022 that’s 38 times as great as in New Zealand.
The difference is down to the vaccination campaigns in these two places. In Hong Kong, at least up to the end of February, the uptake of the booster vaccine was much lower than in New Zealand, and was particularly low in older, more vulnerable age groups. Even second-dose coverage was low in these groups, meaning plenty were at a high risk of severe disease and death.
Did the UK get it right?
My own country, the UK, decided to lift its remaining restrictions earlier this year, even though cases were still high when controls were eased and remain high now. Was this the right thing to do?
There’s no right answer, but given that non-pharmaceutical control measures only delay infections rather than prevent them, such measures should only continue if the benefits of delaying infections outweigh the more general harms to society and human health that come with restricting people’s freedoms. Given the high levels of immunity across the British population that have resulted from high case levels and good vaccine coverage, lifting controls made sense.
There’s also another important point to consider here. It’s been well publicised that the vaccines’ protective effect against catching the virus and developing symptoms wanes more quickly than protection against severe disease and death. However, there’s emerging evidence (still in preprint, so awaiting review by other scientists) that protection against severe disease also wanes with time.
What this means is that delaying infections could result in people getting COVID at a later date when they are more susceptible to getting badly ill. This was predicted in some of the disease modelling of omicron published at the end of last year (also still in preprint). Imposing additional restrictions in December 2021 would have reduced COVID deaths in January 2022, but at the cost of increased deaths in March.
Personally, I would have preferred to wait till the end of March to lift restrictions, so that we were into spring, when respiratory viruses spread less rapidly. That could have reduced the current NHS pressures stemming from staff absences.
And finally, even though lifting controls made sense, today the UK still has a population of older or clinically vulnerable people who have not yet had the virus and whose vaccine immunity is waning. We must focus now on preventing these people from developing severe disease – perhaps through further vaccine boosters or use of antiviral drugs – rather than on attempting to reduce transmission in the general population.
![]()
Paul Hunter consults for the World Health Organization (WHO). He receives funding from the UK National Institute for Health Research, the WHO and the European Regional Development Fund.