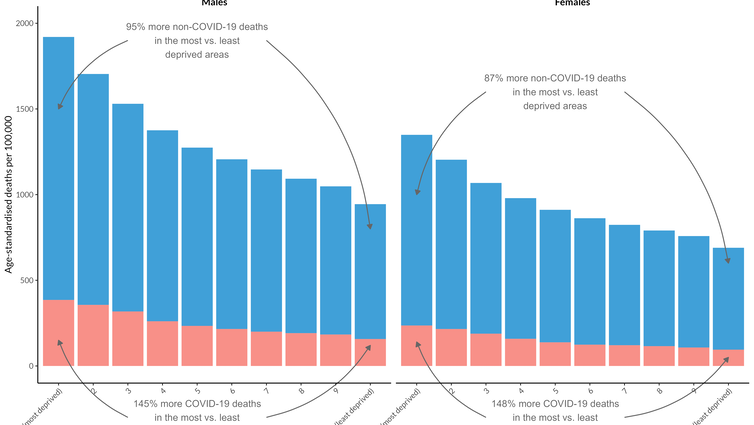
A recurring theme of the pandemic has been how COVID’s impacts have not fallen equally across the UK population. The health and financial burden of the disease has been felt disproportionately by people living in deprived areas.
An example of the starkness of this disparity is the fact that, once you account for age differences between the groups, the most deprived areas in England recorded a COVID mortality rate that was two and a half times higher than the least deprived areas in the first year of the pandemic.
Data from ONS, analysis by Colin Angus
You don’t have to think too hard to come up with some of the causes of this inequality. People from more deprived groups are less likely to have been able to work from home, more likely to live in larger, multi-generational households with less space and poorer ventilation, less likely to have access to good quality healthcare services and more likely to have existing health conditions that increase the risks associated with a COVID infection. These factors already drove significant inequalities in health in the UK, but the pandemic supercharged them.
More recently, however, something unexpected has happened. In late September, rates of new COVID cases, which had stubbornly been highest in the most deprived areas for the previous 18 months, shot up in areas of low deprivation. Suddenly, the inequality in COVID cases reversed without warning.
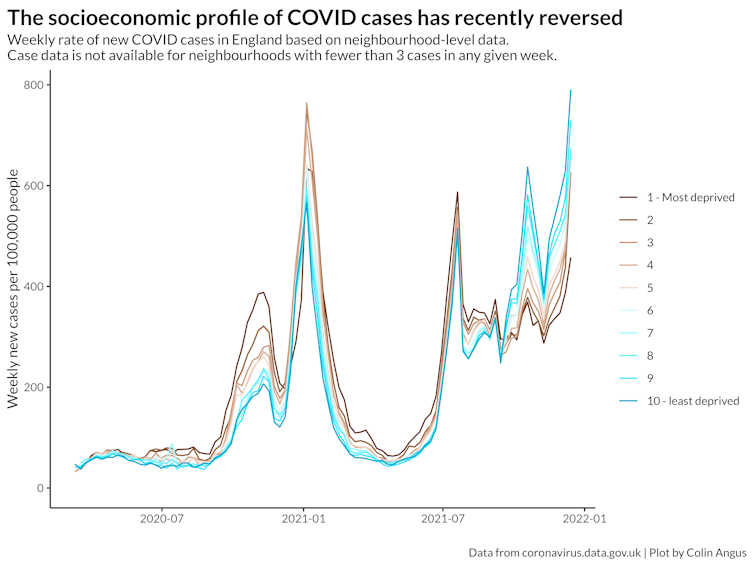
Data from coronavirus.data.gov.uk, analysis by Colin Angus
A big factor in this change was a surge in cases in schoolchildren in the least deprived areas. But the same change occurred in older age groups, too. So what was going on?
There are many possible explanations, but one contributing factor is likely to be the fact that, having had high case rates for so long, more deprived areas had much higher levels of infection-acquired immunity. Essentially, so many people had had COVID already that the virus started to run out of susceptible people to infect. Many more affluent areas, however, had seen relatively fewer cases and so had greater exposure to new outbreaks, particularly among schoolchildren who didn’t have the additional protection of vaccines.
Unfortunately, there has been a major new development since then: omicron has arrived. The new variant appears to be even more infectious than previous variants of concern, and it has some degree of immune escape, which means it is much better at reinfecting people who have some degree of immunity, whether that is through having been infected or being vaccinated.
This ability to reinfect people who have already had COVID means that omicron represents a huge risk to more deprived areas. All of the factors that gave rise to the inequalities in COVID cases and deaths that we’ve seen over the first 18 months of the pandemic are still present.
The fact that omicron can overcome the wall of protection that has been built up in deprived areas through such high levels of prior infection means that there is a risk that these inequalities are going to be repeated in the coming weeks and months. Just when it seemed as though there was a light at the end of the tunnel for many living in deprived areas, the light began to fade.
There is much we still don’t understand about the new variant – whether people infected with it are less likely to end up in hospital than previous variants, for example. But there are reasons to be at least cautiously optimistic on that front. However, even if that turns out to be true, we have already seen unprecedented numbers of cases in young people in London in the past week, and a small percentage of a very big number can still be alarmingly large. Given the huge pressure that the NHS is already under, any increase in hospital admissions is a serious concern.
Boosters need an equitable rollout
The one hope is boosters. The evidence is already clear that a third vaccination is effective against omicron. The government and the NHS are pulling out all the stops to get as many booster jabs in as many arms as possible. But as with the first and second dose rollouts, vaccination rates are lowest in the most deprived areas.
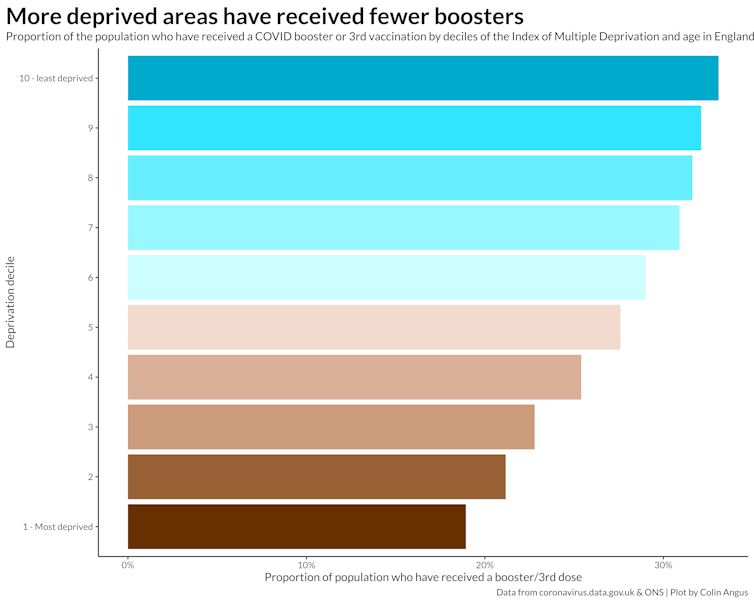
Data from coronavirus.data.gov.uk and ONS, analysis by Colin Angus
If the UK government focuses only on getting as many boosters delivered as possible, without making a real effort to increase vaccination coverage in the most deprived areas, there is a very real concern that the gulf in health between the haves and the have nots in England will further widen.
![]()
Colin Angus does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.