Jacob Lund/Shutterstock
The benefits of breastfeeding are wide-ranging and life-changing. Breast milk contains antibodies that reduce the risk of asthma, allergies, diarrhoea and ear infections. Breastfed infants are hospitalised less frequently than infants who are not. In later life, breastfed children and less likely to be overweight and have higher IQs. And women who have breastfed are at reduced risk of breast and ovarian cancer.
What’s more, these benefits increase with the duration of breastfeeding. Breastfeeding over the first week of life is beneficial, but breastfeeding over the first year is far better.
It’s sensible then that Public Health England has made it a priority to support breastfeeding and that the Scottish government has committed to a goal of increasing breastfeeding duration.
In a recent pilot study, myself and MSc student Tracy McGillivray gave planning/advice cards to some women in the closing stages of their pregnancy to help them manage the transition to breastfeeding. We discovered women who received the cards were four times less likely to quit breastfeeding than women who had not received them.
Myths and misconceptions
Breastfeeding is tough. It is physically gruelling. A majority of the women who answered the large-scale Infant Feeding Survey in 2010 reported that they experienced breast or nipple pain at some point when breastfeeding.
Even these days, it can be socially bruising. Recently I have seen two news stories about women being berated for breastfeeding – in one case the breastfeeding mother was being told to leave her own garden.
And there continue to be misconceptions about breastfeeding. Some of these misconceptions are cultivated by industry. A study published recently found that manufacturers of infant feeding formula gave a skewed impression of the relative merits of formula versus breastfeeding. The manufacturers’ websites underplayed the benefits of breastfeeding and overstated its challenges.
But some of the misconceptions are unfortunate accidents. For example, advocates often claim that breastfeeding is “the most natural thing in the world”. This phrase neglects the fact that for new mothers breastfeeding is a new behaviour that, like all new behaviours, takes some getting used to.
Indications of how tough breastfeeding is are revealed in the Infant Feeding Survey. In Scotland, one in five mothers who started breastfeeding stopped just two weeks after birth. Drop-off in those first two weeks is even higher in Wales and in Northern Ireland. Crucially, 86% of mothers who dropped breastfeeding in those first two weeks report that they would have liked to have breastfed for longer.
These statistics – far higher rates of drop-off than women would have wished for themselves – imply that a supportive way of helping women breastfeed more successfully is needed. Tracy McGillivray, an MSc student on our behavioural science course who also works as as a child nutrition specialist with NHS Lothian, came up with one such idea – and now we know it works.
She identified the gap between intention and reality described in the previous paragraph and worked with me on designing a breastfeeding planning card. She recruited 81 women at antenatal classes around Edinburgh and randomly assigned some mothers to serve as a control group who did not receive a card, and others to receive one of two planning cards we designed.
What did the cards say?
One goal for the planning card was to help women anticipate some of the challenges they would face in those early days after birth when establishing a breastfeeding routine. We also wanted to reassure women that it is normal to experience difficulty breastfeeding. So we listed on one side of the card four obstacles to breastfeeding commonly cited by women.
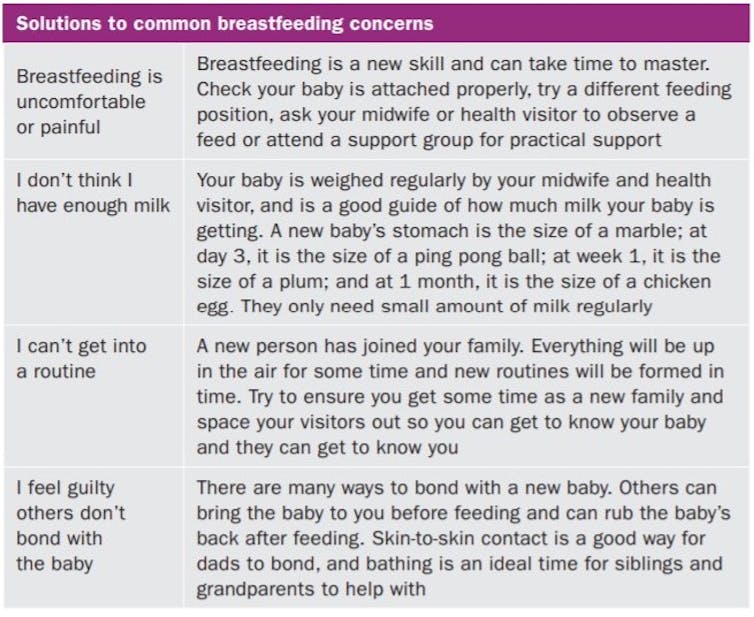
Author provided
A second goal for the card was that it would help women plan to meet those challenges. The card was given to women in the closing stages of their pregnancy – at a moment when the reality of becoming a mother was imminent but when there remained time to take action to prepare for breastfeeding. We provided alongside the list of obstacles a list of related tips taken from the Infant Feeding Survey and peer-reviewed literature. We called the resulting card the Obstacles/Tips card, or O/T card in the graph below.
In addition, some cards featured on their reverse side a prompt that read: “When I have my baby, I intend breastfeeding for …” We added this because research on dieting and exercising shows that deliberately articulating a specific intention helps people achieve their health goals. In the graph we call these the “Enhanced O/T card”.
David Comerford, Author provided
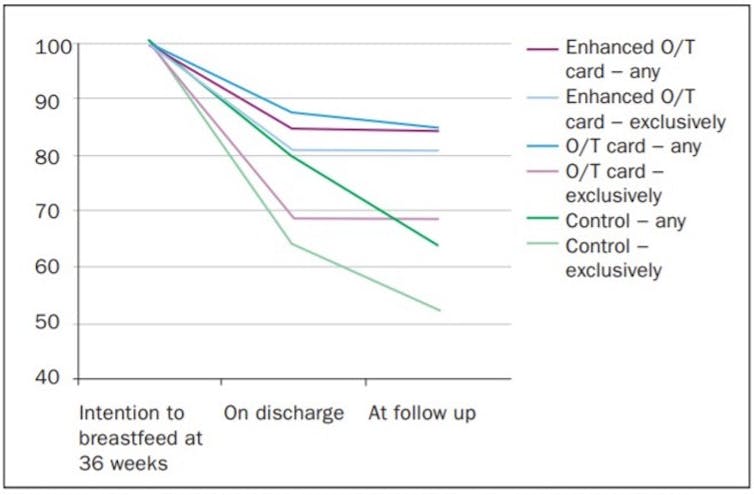
The graph above shows what happened. The green lines depict the control group of women who received no card. All had expressed an intention to breastfeed. On discharge from hospital, 80% of them were actually breastfeeding. When we contacted them 10-14 days after their due date, just 64% were still giving their baby any breast milk. The negative trend also occurs among this control group if we focus on exclusive breastfeeding, meaning no topping up with formula milk. This result is important because babies who are exclusively fed breastmilk enjoy particular health benefits.
Contrast those downward trends in breastfeeding and exclusive breastfeeding with the two card groups. The vast majority of mothers who were breastfeeding on discharge from hospital in both the O/T card and the Enhanced O/T card groups were still breastfeeding 10-14 days later.
The difference in slope over the discharge to follow up period – a downward drop for the control group versus a near horizontal line for the card groups – is striking. Given the substantial benefits of breastfeeding, we hope these results encourage others to adopt and adapt our card to promote breastfeeding.
![]()
David Comerford receives funding from UKRI on research around Covid-19.











