Krakenimages/Shutterstock
A close friend – let’s call him John – recently called, asking for advice. He woke up with severe muscle aches and fatigue. Understandably worried that it could be COVID-19, he asked whether he should go to work, run to get a test or stay home. Because he didn’t have other symptoms, such as a fever, cough or shortness of breath, he was unsure what to do. Of course, this could be any other respiratory infection, such as the flu or the common cold, but what if it is COVID-19? What is the risk of him transmitting the virus to others?
To understand when people with COVID-19 are most likely to be infectious, our team conducted a study which was recently published in The Lancet Microbe.
We investigated three things: viral load (how the amount of the virus in the body changes throughout infection), viral shedding (the length of time someone sheds viral genetic material, which does not necessarily mean a person is infectious), and isolation of the live virus (a better indicator of a person’s infectiousness, as the live virus is isolated and tested to see if it can replicate in the laboratory).
We found that viral load reached its peak in the throat and nose (which is thought to be the main source of transmission) very early in the disease, particularly from the first day of symptoms to day five of symptoms – even in people with mild symptoms.
We also found that genetic material can still be detected in throat swab or stool samples for several weeks. But no live virus was found in any sample collected beyond nine days of symptoms. Although some people, especially those with severe illness or with a weakened immune system (say from chemotherapy), may have longer viral shedding, the results suggest that those infected with SARS-CoV-2 are most likely to be highly infectious a few days before symptoms start and the following five days.
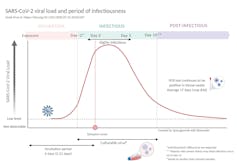
In comparison, the viral load of Sars peaks at 10-14 days and for Mers at 7-10 days after symptoms start (Sars and Mers are both diseases caused by coronaviruses). This explains why the transmission of these viruses was effectively reduced by immediately finding and isolating people who had symptoms. It also explains why it has been so difficult to contain COVID-19 as it spreads very quickly early in the disease course.
Contact tracing and modelling studies also show that transmission is highest in the first five days of experiencing symptoms. According to a recent study, the period of highest infectiousness is within about five days of symptoms starting. A contact tracing study from Taiwan and the UK found that most contacts got infected if they were exposed to the infected person within five days of their symptom onset.
By the time most people get their test result, they may already be beyond their most infectious period. This early viral load peak suggests that to prevent onward transmission, a person with COVID-19 needs to self-isolate as soon as symptoms start without waiting for test results.
John self-isolated immediately and called everyone that he had been in contact with in the previous few days. The next day, he woke up with a mild fever. He couldn’t get a test immediately, but was able to get an appointment at a later time. The results were available by day five of his symptoms. He tested positive for COVID.
Fortunately, John managed to self-isolate throughout his most infectious period and his contacts started quarantining immediately.
John was fortunate in that he was able to work from home and continue to get paid. But according to a UK survey, only one in five people are able to self-isolate. Barriers include having a dependent child at home, having low income, experiencing greater financial hardship during the pandemic, and being a key worker, such as a nurse or teacher.
Governments could do more to help
How will a diagnosis help if your living situation doesn’t allow for isolation, if you have a job that can’t be done from home, and your work doesn’t provide sick leave? And how will a diagnosis help if your family depends on your income to meet basic needs, or your access to care is linked to your employment?
This highlights why we must focus on supporting people with COVID-19 to self-isolate early in the disease course. Here are four ways to help people self-isolate:
- Income relief to avoid undue pressure to work when sick (the proportion of salary covered by sick pay is 29% in the UK).
- Housing for disadvantaged communities, especially those living in crowded houses and those living with vulnerable people, as has been successfully done in Vermont, in the US.
- Services to support people who are self-isolating, as is done in New York and many south-east Asian countries.
- Remove barriers to accessing healthcare and consider making isolation periods shorter – five to seven days after symptoms begin. This could cover the most infectious period and might improve people’s ability to comply with isolation. In September, France dropped isolation period for cases to seven days, and Germany is considering shortening it to five days. The benefit of shortening isolation may more than offset any risk to the community.
With these measures in place, we should be in a much better position to beat the pandemic.
![]()
Müge Çevik receives COVID-19 research funding from Chief Scientist Office and UKRI-Grand Challenges Research Fund.
Antonia Ho receives COVID-19 research funding from UKRI, Wellcome Trust, Chief Scientist Office, and the Scottish Funding Council Grand Challenges Research Fund.











