Thirty years ago dementia was a condition less understood than it is now and assumed to be a normal part of ageing. A condition which affects the memory, it can also affect sight, hearing, balance, walking, visual and spatial understanding, navigation and tonal differentiation, and can cause hallucinations.
Today, dementia affects approximately 50 million people worldwide and is predicted to double in 20 years due to an ageing population and an increase in awareness and diagnosis. Dementia has become a global issue.
The design of the built environment can have a profound impact on how a person with dementia perceives, experiences and engages with the places and spaces in which they live. Yet much of the design guidance currently available is underpinned by research undertaken in developed countries.
Research has shown that rather than drawing upon the experiences of older people, their families and care professions, architects designing for later life are more likely to draw upon presumed needs and experiences of the older person as imagined by themselves.
This begs the question of who will lead the global challenge to ensure spaces and buildings support this increase in the prevalence of dementia while retaining all the beauty, joy and quality of life that good architecture and design can bring.
Dementia design principles
Dementia design is a non-medical approach to help reduce some of the symptoms associated with dementia, such as agitation, aggression, confusion, incontinence and visual, spatial and navigational difficulties.
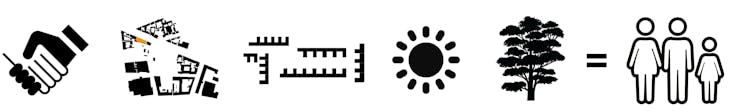
The international consensus on principles agrees that dementia design should incorporate the following concepts: it should compensate for disability, maximise independence and enhance self-esteem and confidence. It should also demonstrate care for staff needs, be orientating and understandable, reinforce personal identity, welcome relatives and the local community, and allow control of stimuli – for example, reducing unwanted noises associated with alarm systems.
Dementia design principles came into being in the late 1980s when the development of Confused and Disturbed Elderly (CADE) units in New South Wales, Australia, established a design brief which advocated for specific principles to support those living with dementia. Soon after, the Dementia Services Development Centre (DSDC) was established at the University of Stirling, which became influential in this field.
Lesley Palmer, Author provided
At the time, leaders in this field called on architects to consider dementia not as a disease, focusing design on spaces that support physical decline, but rather as a disability where the design focus shifts to spaces that can maintain everyday functions of people living with dementia. The importance of this juxtaposition should not be underestimated and is better understood in the context of the seismic shift that was happening in built environment legislation in the UK.
The Disability Discrimination Act of 1995 (DDA) placed an obligation on spaces to be free from discrimination – the environment being the disabling factor affecting opportunities to participate in everyday life. The new act resulted in a wholescale review of how the built environment supported – or didn’t – those with physical impairments.
Architecture and the codes which govern it were redesigned. Proponents of dementia design witnessed this and lobbied for this approach to include people living with dementia, but there has been very little progress on this issue until recently.
Dementia design today
Developments in dementia research recognise that the condition is not a natural part of ageing, but that the risk of developing it increases with age. Alcohol, smoking, cholesterol and diabetes also increase the risk of dementia, and air pollution has been also identified as impacting on brain health.
There is an increasing global interest in the adoption of dementia design principles. Alzheimer’s Disease International has dedicated its World Alzheimer Report 2020 to dementia-related design, and policymakers are working to embed the evidence into environmental guidelines.
There is also a growing call for intergenerational living and dementia design principles are being integrated into age-friendly projects such as retirement living and community buildings.
For the most part this is encouraging. An age-friendly city could foster healthy and active ageing by building and maintaining that capacity across the course of people’s lives. It could support the development of healthy brain function from early years, help people maintain cognition through their later years and support cognitive decline as people age.

Shutterstock
A public health issue
Thinking ahead and considering the complex causal factors, increased diagnosis rates and multi-disciplinary scope of dementia therapies, people living with the condition and their families would benefit from a coordinated global response in every country and across all cultures. Early proponents of dementia design advocated for dementia to be considered as a disability which required spaces that maintain function. I believe it would also be helpful to recognise dementia as a public health issue and use design to address some of the challenges this brings.
This would enable architects and planners to integrate dementia-design principles in a similar fashion to the way in which the Disability Discrimination Act supported people with physical disabilities. They could employ the tools of health impact assessment to plan places to support prevention by reducing the risk of developing some of the underlying health conditions mentioned earlier. The provision of green spaces, active travel and play, walkable neighbourhoods, improved biodiversity and air quality could all help the fight against dementia.
To fully understand the benefits, there is a pressing need for critical discussion and further research and architectural projects with briefs which challenge designers to address this important global issue.
Acknowledging more than 30 years of dementia design, Stirling University’s Dementia Services Development Centre has launched Architecture for Dementia: 2008-2020 – a unique selection of outstanding projects from across the globe. Each one has received a DSDC “Stirling gold” for dementia-friendly buildings.
If there was ever a time to celebrate evidence-based dementia design, it is now. This record will stand as a baseline for the development of the next 30 years of progress in the design of dementia-inclusive design and help improve the quality of life for millions of people around the world living with this debilitating condition.
![]()
Lesley Palmer works for the DSDC, University of Stirling. In her role at the DSDC, University of Stirling she receives funding from research council grant and consultancy services by third party organisations. She is affiliated with INCH Architecture & Design Ltd.











