Numstocker/Shutterstock
A vaccine against COVID-19 is urgently needed if we’re to stop the virus spreading and prevent potentially millions of further deaths. We’re now one step closer to that goal.
Today, we published early results from our clinical trial of the vaccine ChAdOx1 nCoV-19 (also known as AZD1222), designed by the University of Oxford and developed in partnership with AstraZeneca. The preliminary data shows that it is safe and induced a strong antibody response in all vaccinated volunteers, suggesting that an effective vaccine could be within reach.
This trial was the first time that the vaccine had been given to humans: 543 healthy adults aged 18-55 were vaccinated with a single dose of ChAdOx1 nCoV-19. A further 534 people were given a control vaccine that gives similar minor reactions, including injection site redness and mild pain. Volunteers are having their immune response (both antibodies and T cell levels) monitored for at least 12 months, and will also be observed to see whether or not they develop COVID-19.
The preliminary data from the trial clearly demonstrates that the vaccine induces an antibody response within 28 days. This response is in a similar range to that in individuals who have recovered from COVID-19, providing encouragement that the vaccine will be able to protect the majority of people against infection.
Ten volunteers were also given a second “booster” dose of the vaccine. This increased the antibody response to even higher levels, and 100% of blood samples from this group showed neutralising activity against COVID-19 infection in a laboratory setting.
The vaccine also induced T cells that specifically recognise SARS-CoV-2, the virus that causes COVID-19. It’s encouraging to see both antibody and T cell responses, as together this is the right kind of immune response that could lead to protection against the virus. Importantly, the vaccine demonstrates an acceptable safety profile, with no vaccine-induced severe adverse events – that is, no major side-effects.
We were confident testing the vaccine in humans after encouraging trials with mice and rhesus macaque monkeys. These had shown that the vaccine was safe and induced a robust immune response. Significantly, the vaccinated monkeys were protected from severe disease after they were challenged with a much higher dose of SARS-CoV-2 than humans would encounter through natural exposure.
How does this vaccine work?
Vaccines work by training the immune system to recognise and fight off infectious agents (pathogens), such as bacteria and viruses. Vaccines do this by presenting the immune system with a readily identifiable part of a pathogen, which the immune system remembers so that it can quickly respond should it encounter that same pathogen in the future.
Most vaccines in development for SARS-CoV-2 – including this one – focus on presenting the spike protein that decorates the surface of the virus. It’s this protein that allows the virus into human cells by binding to a molecule on their surface called ACE2.
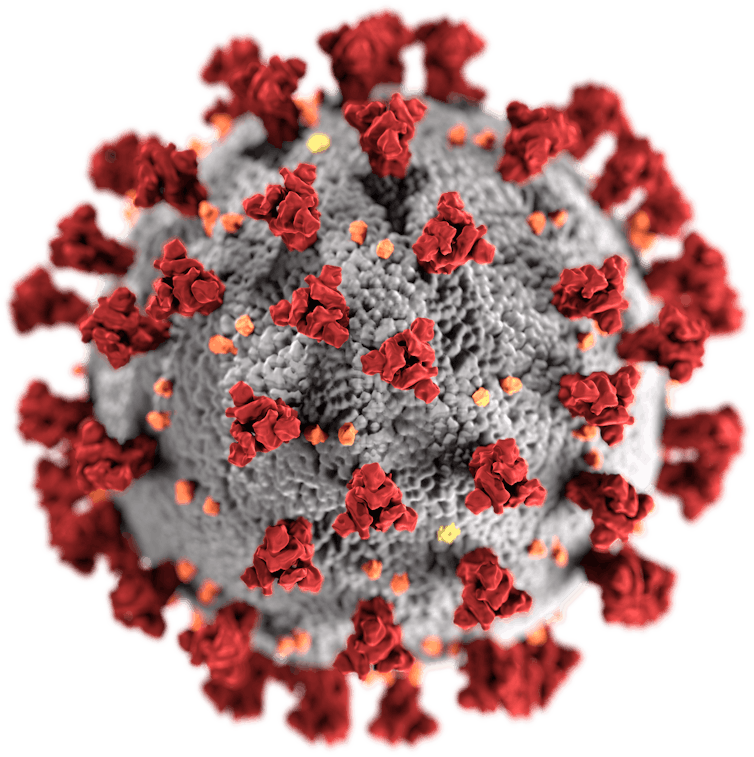
US Centers for Disease Control and Prevention/Wikimedia Commons
There is a broad range of approaches to vaccine design; ChAdOx1 nCoV-19 is what’s known as a viral vector vaccine. To make this vaccine, particles of a different, harmless virus (called ChAdOx1) are loaded with the portion of SARS-CoV-2 DNA that instructs cells how to build the spike protein.
When these ChAdOx1 particles infect human cells, the coronavirus DNA is then “expressed”, building the spike protein for the immune system to respond to. Importantly for vaccine safety, the viral vector can’t replicate and cause an ongoing infection.
The ChAdOx1 viral vector has been used to make eight vaccines already in clinical trials for other human diseases, including Mers (Middle Eastern respiratory syndrome), a coronavirus that is related to SARS-CoV-2.
What happens now?
Crucially, we need to demonstrate that the vaccine is effective – that it results in significantly lower (ideally zero) cases of COVID-19 in the ChAdOx1 nCoV-19 vaccinated group versus the control group. Falling infection rates in the UK are an excellent outcome for the health of the nation, but may compromise the ability to show this.
If there are no cases of COVID-19 in the group receiving the control vaccine, comparing that group to the vaccinated group would be meaningless. Deliberately infecting people with the virus may be possible in future (after careful consideration of the ethical implications), but is not currently allowed.
For this reason, a second trial has been launched in approximately 10,000 UK individuals, focusing on health workers, and further trials are being conducted in Brazil and South Africa, where infection rates are much higher. The expanded UK trial will include children and older adults to estimate vaccine efficacy in these age groups. Immune responses in people over 70 are often lower than those in younger adults.
It’s essential to follow the vaccine-induced immune response over a period of at least one year, to estimate whether booster injections will be required, and if so how often. My personal prediction – based on decreases in antibody levels in individuals infected with other types of coronavirus, rather than data from the current vaccine trial – is that we’re likely to need yearly boosters, similar to annual flu jabs.
Finally, if the vaccine proves effective, rapid manufacture of potentially billions of doses would be required to supply the world. To facilitate this, AstraZeneca has already initiated a large-scale vaccine manufacturing programme, aiming to have hundreds of millions of doses with delivery starting by the end of 2020. Agreements are in place to provide the vaccine to low-income and middle-income countries and also to the UK, Europe and the US.
![]()
Rebecca Ashfield consults for SpyBiotech Ltd and OSI (Oxford Science Innovation) although these organisations will not benefit from this article. She is CSO of Ducentis Biotherapeutics Ltd, which develops novel therapies for autoimmune diseases and inflammation.











